1. Definition
What is a Surgical Shadowless Light (OT light)?
A Surgical Shadowless Light, commonly known as an Operating Theatre (OT) Light or Surgical Light, is a specialized medical device designed to illuminate the surgical site with intense, focused, and homogenous light. Its primary function is to provide surgeons with a clear, detailed, and shadow-reduced view of the operative field during surgical procedures. Unlike standard lights, which cast sharp shadows from the surgeon’s hands and instruments, an OT light is engineered to minimize these obstructions, thereby enhancing precision and reducing eye strain for the surgical team.
How it works:
The fundamental working principle is multi-source point lighting combined with optical design. A typical shadowless light consists of several individual lamp modules (often halogen, LED, or a combination) arranged in a ring or configuration within a single head. Each module emits light from a slightly different angle towards a common focal point (the surgical site). The overlapping of these multiple light beams from different directions “fills in” the shadows created by any single source. When a hand or instrument blocks one light path, the other beams from different angles continue to illuminate the area, drastically reducing the shadow’s density. Advanced models incorporate reflectors, lenses, and filters to further control light spread, depth of illumination, and color temperature.
Key Components:
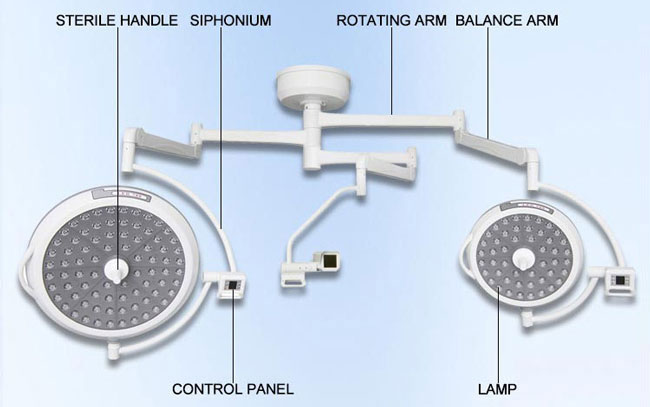
- Light Head: The main assembly containing the light sources (LED arrays, halogen bulbs). It is often designed with a concentric or modular pattern.
- Arm System: A series of articulated arms (usually ceiling-mounted via a track or a single pendant) that allow precise, friction-free positioning of the light head. Arms have multiple joints for extensive mobility and stability.
- Control Panel/Interface: Buttons, touchscreens, or handles (often sterile) for adjusting light intensity, color temperature, focus (spot size), and sometimes programmed settings.
- Central Control Unit/Driver: The electronic system that regulates power to the light sources, manages thermal output, and controls dimming functions.
- Mounting System: Ceiling tracks, pendants, or mobile floor stands that provide structural support.
- Sterile Handle Covers: Disposable or autoclavable sleeves that allow the surgeon to reposition the light head during a procedure without breaking sterility.
- Camera Port/Interface (in some models): An attachment point for integrating surgical cameras and recording systems.
2. Uses
Clinical Applications:
OT lights are indispensable across the entire spectrum of invasive procedures:
- General & Abdominal Surgery: Providing deep-cavity illumination for laparotomies, hernia repairs, etc.
- Cardiothoracic & Neurosurgery: Offering precise, high-intensity light for highly delicate operations on the heart, lungs, brain, and spine.
- Orthopedic Surgery: Illuminating deep joint spaces during hip/knee replacements and spinal fusions.
- Trauma & Emergency Surgery: Delivering immediate, high-output light for uncontrolled, critical situations.
- Minimally Invasive Surgery (Laparoscopy/Endoscopy): While these procedures use internal cameras, OT lights are crucial for port placement, auxiliary incisions, and open conversions.
- Obstetrics & Gynecology: Used in C-sections, hysterectomies, and other pelvic surgeries.
- Ophthalmic, ENT, and Plastic Surgery: Providing focused, shadow-reduced light for intricate work on small, sensitive anatomical areas.
Who uses it:
- Surgeons and Surgical Assistants (primary users)
- Scrub Nurses and Circulating Nurses
- Anesthesiologists (for procedures like central line placement, if the main light is shared)
- Surgical Technologists
Departments/Settings:
- Main Operating Rooms (ORs)
- Day Surgery/Ambulatory Surgery Centers
- Labor & Delivery Suites
- Emergency Department Trauma Bays
- Special Procedure Rooms (e.g., in Cath Labs, Interventional Radiology)
- Intensive Care Units (ICUs) for bedside procedures
- Veterinary Operating Theaters
3. Technical Specs
Typical Specifications:
- Illuminance (Lux): 40,000 to 160,000+ lux at 1 meter (core focus). Modern standards often target > 40,000 lux.
- Light Field Diameter: Adjustable, e.g., from a focused spot of 15 cm to a wide field of 30+ cm at 1m distance.
- Color Rendering Index (CRI): >85, with >90 ideal for true tissue differentiation. Sunlight has a CRI of 100.
- Color Temperature (Kelvin): Adjustable, typically between 3000K (warm/yellow) and 5000K (cool/white, simulating daylight). 4000K-4500K is often preferred.
- Depth of Illumination: Ability to provide adequate light even at deep cavity levels (e.g., >20cm).
- Shadow Reduction: Quantified as a percentage; high-end lights achieve >98% shadow dilution.
- Heat Management: Surface temperature rise at the light head should be minimal (<2°C at the handle, per IEC 60601-2-41 standard).
Variants & Sizes:
- Single-Headed: Most common, with one light head on an arm system.
- Double-Headed (Dual Ceiling Mount): Two independent light heads on separate arms, often used for major surgeries for backup and combined illumination.
- Multi-Spot Systems: Multiple smaller heads on a single mounting, common in dental or minor procedure settings.
- Mobile/Floor Stand: For clinics, minor ORs, or as backup.
Materials & Features:
- Materials: Light heads use high-grade polymers and metals (anodized aluminum, stainless steel) for easy cleaning. Arms are typically aluminum alloy.
- Key Features:
- LED Technology: Now standard. Offers long life (~50,000 hrs), low heat, energy efficiency, and stable color temperature.
- Touchless Control: Infrared or sensor-based controls for non-sterile adjustment.
- Camera Integration: “Beam-splitter” technology to integrate a camera without losing light output.
- Sterile Handle Remote Control: Buttons on the sterile handle for intensity/focus.
- Emergency Power: Battery backup to maintain light for a set period during power failure.
- Focus Memory: Pre-set lighting programs for different surgery types.
Models (Notable Examples):
- Dräger Polaris 700 / 900
- STERIS Harmony LED 600 / iLX
- Berchtold Chromophare / Novalume
- Maquet PowerLed / Misha
- Skytron 6500SL / Ultralume
- Getinge Pled / Mera 400
4. Benefits & Risks
Advantages:
- Enhanced Visual Acuity: Critical for identifying tissue planes, vessels, and nerve structures.
- Reduced Surgeon Fatigue: Minimizes eye strain and mental effort to see around shadows.
- Improved Surgical Precision & Safety: Directly contributes to fewer errors and better patient outcomes.
- Sterility Maintenance: Easy-to-clean surfaces and sterile handles prevent contamination.
- Flexibility & Stability: Arms allow easy repositioning and then stay firmly in place.
- Energy Efficiency (LED): Lower power consumption and reduced HVAC load from heat.
Limitations:
- Cost: High-quality OT lights represent a significant capital investment.
- Physical Space: Ceiling-mounted systems require specific OR layout planning.
- Learning Curve: For advanced features and programming.
- Potential for Glare: If not properly aligned or if reflective instruments are used.
Safety Concerns & Warnings:
- Thermal Injury: Although minimal with LEDs, prolonged close proximity of any light source to tissue or drapes can cause burns.
- Mechanical Failure: Risk of arm drift or, in extremely rare cases, detachment if not properly maintained.
- Electrical Safety: Must be installed and grounded per hospital electrical codes.
- Infection Control: If the housing or handles are not properly cleaned between procedures.
Contraindications:
There are no direct medical contraindications for the device itself. The “contraindication” relates to its environment: it should not be used in an explosive atmosphere (unless specifically rated for such) or with damaged components (cracked housing, frayed cables).
5. Regulation
Surgical lights are regulated as critical medical devices.
- FDA Class: Class II (moderate to high risk). Requires 510(k) premarket notification to demonstrate substantial equivalence to a predicate device.
- EU MDR Class: Class IIa (for non-central circulatory/ nervous system illumination) or Class IIb (if intended to illuminate central circulatory/ nervous system during life-threatening surgery), per Rule 10.
- CDSCO Category (India): Class C (Moderate to High Risk), requiring a license from the Central Licensing Authority.
- PMDA Notes (Japan): Regulated as Class II under the Pharmaceutical and Medical Device Act (PMD Act). Requires certification from a Registered Certification Body.
- ISO/IEC Standards:
- ISO 80601-2-41: The paramount standard for basic safety and essential performance of surgical lights.
- IEC 60601-1: General standard for medical electrical equipment safety.
- ISO 9680: Dentistry – Operating lights (specific variant).
6. Maintenance
Cleaning & Sterilization:
- Daily/Post-Procedure: Wipe down the light head, arms, and handles with a hospital-grade, low-level disinfectant (e.g., alcohol-based or quaternary ammonium compound). Do not spray directly; spray onto a cloth.
- Sterile Handles: Use disposable sterile handle covers for each procedure. Reusable handles must be sterilized (autoclaved) per manufacturer instructions.
- Avoid: Harsh abrasives, bleach-based cleaners, or solvents that can damage coatings and plastics.
Reprocessing: Primarily refers to the sterilization of reusable handle components. Follow the validated cycle (e.g., steam autoclave at 121°C for 20 mins) as per the device manual.
Calibration:
- Light Intensity & Color: Should be checked annually or as per manufacturer schedule using a calibrated lux meter and color temperature meter.
- Mechanical Balance: Check for arm drift or instability. Adjust friction brakes or counterbalance mechanisms as needed.
Storage:
- When not in use, position the light head against its ceiling stop or parking brake.
- Store mobile lights in a dry, clean area.
- No specific temperature/humidity requirements beyond standard OR conditions.
7. Procurement Guide
How to Select the Device:
- Assess Clinical Needs: Consider the types of surgeries performed (cardiac vs. general), OR size, and surgeon preferences.
- Evaluate Lighting Performance: Request a live demonstration. Check for true shadow reduction, depth of illumination, and color quality on a simulated cavity.
- Test Maneuverability: The arm should move smoothly with one finger, stay in position without drift, and have a sufficient reach.
- Consider Integration: Does it need to interface with your OR integration/surgical video system?
- Review Maintenance & Service: Understand service contract costs, part availability, and local technical support.
Quality Factors:
- Illumination Performance (Lux, CRI, Shadow Reduction)
- Build Quality & Stability of the arm system
- Ease of Cleaning (seamless surfaces, few crevices)
- Reliability & Warranty (typically 3-5 years on LEDs)
- Vendor Reputation & Support
Certifications: Look for CE Marking (for EU), FDA 510(k) Clearance (for US), and compliance with ISO 80601-2-41.
Compatibility: Ensure the mounting system (track or single point) is compatible with your OR ceiling structure. Verify camera/video interface compatibility if needed.
Typical Pricing Range:
- Basic LED Single Head (Mobile): $5,000 – $15,000
- Standard Ceiling-Mounted LED Single Head: $15,000 – $30,000
- High-End / Dual Head Ceiling System: $40,000 – $80,000+
(Prices vary widely based on features, brand, and region.)
8. Top 10 Manufacturers (Worldwide)
- STERIS (USA): A global leader in infection prevention. Notable line: Harmony LED series.
- Getinge (Sweden): Major player in surgical and ICU equipment. Notable line: Pled and Mera.
- Dräger (Germany): Renowned for critical care and OR solutions. Notable line: Polaris series.
- Maquet (Subsidiary of Getinge, Germany): Specializes in surgical workplaces. Notable line: PowerLed.
- Berchtold (USA/Germany): A Stryker company, historically a pioneer in OT lights. Notable line: Chromophare and Novalume.
- Skytron (USA): Known for OR tables, lights, and booms. Notable line: 6500SL and Ultralume.
- Hillrom / Baxter (USA): Provides a wide range of hospital equipment, including surgical lights (part of their capital equipment portfolio).
- Simeon Medical (Germany): Specialized in high-quality surgical lights and OR integration.
- Brandon Medical (UK): A key UK-based manufacturer of surgical lights and OR integration systems.
- Mindray (China): A rapidly growing global provider of medical devices, including a range of surgical lights for cost-conscious markets.
9. Top 10 Exporting Countries (Latest Year – Based on HS Code 940540: “Lighting Fittings for Medical Use”)
Rankings are illustrative based on recent global trade data trends.
- Germany: Leading exporter of high-end, precision-engineered surgical lights.
- United States: Major exporter, home to several top manufacturers.
- China: Dominant exporter of mid-range and economical models, with growing quality.
- Mexico: Significant exporter, often as a manufacturing hub for North American companies.
- Netherlands: Key European trade and distribution hub for medical devices.
- United Kingdom: Home to niche manufacturers and a strong re-export market.
- France: Exporter of specialized medical equipment, including OT lights.
- Italy: Known for design and engineering in medical lighting.
- Sweden: Home to Getinge, a major global player.
- Japan: Exporter of high-quality, technologically advanced devices, primarily within Asia.
10. Market Trends
Current Global Trends:
- Full LED Adoption: The shift from halogen/xenon to LED is nearly complete in developed markets.
- Integration & Connectivity: Lights are becoming nodes in the “smart OR,” connecting to control panels, video systems, and hospital networks for data on usage and maintenance.
- Ergonomics & Hygiene: Focus on even easier-to-clean designs and touchless control to support infection prevention protocols.
New Technologies:
- Adjustable Color Spectrum: Lights that can shift from cool to warm white or even enhance specific tissue contrasts (e.g., oxygen saturation in vessels).
- AI-Assisted Positioning: Auto-follow or pre-programmed lighting scenes that adjust based on the phase of surgery.
- 4K/HDR Camera Integration: Built-in ultra-high-definition cameras with minimal light loss.
Demand Drivers:
- Rising volume of surgical procedures globally.
- Construction and modernization of hospitals and ASCs (Ambulatory Surgical Centers).
- Increasing emphasis on reducing surgical site infections (SSIs) via better OR hygiene.
- Surgeon demand for improved visualization to support complex, minimally invasive techniques.
Future Insights:
The future points towards the “Context-Aware Surgical Light.” It will integrate with patient imaging data (MRI/CT), automatically adjusting the light field to the specific anatomy. It may also provide real-time visual overlays (via augmented reality) on the surgical field and further reduce physical contact through advanced gesture control.
11. Training
Required Competency:
- Clinical Users (Surgeons/Nurses): Must be trained on safe operation: positioning, adjusting intensity/focus, using sterile handles, and understanding basic troubleshooting (e.g., what to do if light doesn’t turn on).
- Biomedical/Clinical Engineering Staff: Require in-depth training on preventative maintenance, calibration, electrical safety checks, and advanced repairs.
Common User Errors:
- Forcing the Arm: Pushing or pulling on the light head instead of using the handles, potentially damaging the friction mechanisms.
- Improper Cleaning: Using corrosive chemicals or spraying directly onto the light, leading to damage or electrical issues.
- Ignoring Sterile Handles: Touching the light head directly with sterile gloves, contaminating it.
- Incorrect Positioning: Placing the light too far away (reducing intensity) or too close (creating glare and heat risk).
Best-Practice Tips:
- Position First: Move the light into the general position before scrubbing in.
- Use the Focus: Adjust the field diameter to just larger than the incision for optimal illumination and contrast.
- Check Backup Battery: Ensure the emergency power system is tested regularly as part of OR safety checks.
- Partner with Biomed: Report any flickering, unusual noise, or arm drift immediately.
12. FAQs
1. How often do the LED bulbs need to be replaced?
LEDs have an extremely long lifespan (typically 50,000 hours). For average OR use, this can mean 10+ years before any noticeable depreciation. They are not typically “replaced” like halogen bulbs but may require a full module change if they fail.
2. Can an OT light cause burns on a patient?
The risk is very low with modern LED lights due to their minimal infrared (heat) emission. However, prolonged, direct, close contact with any light source on a single spot, especially on sensitive tissue or through moist drapes, should be avoided as a precaution.
3. Why is the Color Rendering Index (CRI) important?
A high CRI (≥90) ensures that the colors of tissues, blood, and organs are rendered accurately. This helps surgeons distinguish between subtle differences (e.g., a pale ischemic intestine vs. healthy pink tissue), which is critical for decision-making.
4. What is the difference between “shadow reduction” and “shadow elimination”?
True shadow elimination is physically impossible. “Shadowless” lights achieve shadow reduction or dilution (often >98%) by overlapping multiple light beams, making the remaining shadows so faint they are functionally irrelevant.
5. What should we do during a power failure?
Modern OT lights have built-in battery backups (UPS). They should automatically switch to battery power, providing reduced but adequate light for a defined period (e.g., 30-60 minutes) to allow safe termination or continuation of the surgery.
6. Is it safe to use a mobile OT light in a regular room?
Yes, mobile lights are designed for this purpose. Ensure the room’s electrical outlets are properly grounded and the floor is level to prevent the stand from tipping.
7. How do we prevent the light head from drifting during surgery?
This is usually a sign that the arm’s friction brakes or counterbalance needs adjustment. This is a maintenance task for your clinical engineering department. Do not attempt to fix it during a procedure.
8. Can we attach our own camera to any OT light?
Not optimally. For best results, use a light with a dedicated camera port or a beam-splitter accessory designed by the manufacturer. Attaching a camera externally often blocks light and provides a poor angle.
13. Conclusion
The Surgical Shadowless Light is far more than a simple lamp; it is a cornerstone of modern surgical practice, a precision tool that directly impacts patient safety and surgical success. From its core principle of multi-source lighting to the latest advancements in LED technology and smart OR integration, the evolution of the OT light reflects the ongoing pursuit of excellence in the operating room. A thorough understanding of its selection, operation, and maintenance is essential for healthcare institutions to ensure they provide their surgical teams with the best possible visualization, ultimately leading to improved clinical outcomes. Investing in a high-quality OT light and the knowledge to use it effectively is an investment in the very foundation of safe and successful surgery.
14. References
- International Electrotechnical Commission (IEC). IEC 60601-2-41: Particular requirements for the basic safety and essential performance of surgical luminaires and luminaires for diagnosis.
- International Organization for Standardization (ISO). ISO 80601-2-41: Medical electrical equipment — Part 2-41: Particular requirements for the basic safety and essential performance of surgical luminaires and luminaires for diagnosis.
- U.S. Food and Drug Administration (FDA). Device Classification Database.
- European Commission. Medical Device Regulation (MDR) 2017/745.
- Healthcare Information and Management Systems Society (HIMSS). Interoperability and the Smart OR.
- Surgical Light Manufacturer Technical Manuals (STERIS, Getinge, Dräger).
- Journal of Clinical Engineering & Surgical Endoscopy (Various issues on visualization technology).
- World Health Organization (WHO). Global Guidelines for the Prevention of Surgical Site Infection. (Highlights the role of the environment, including lighting hygiene).