1. Definition
What is a Biosafety Cabinet (Class II)?
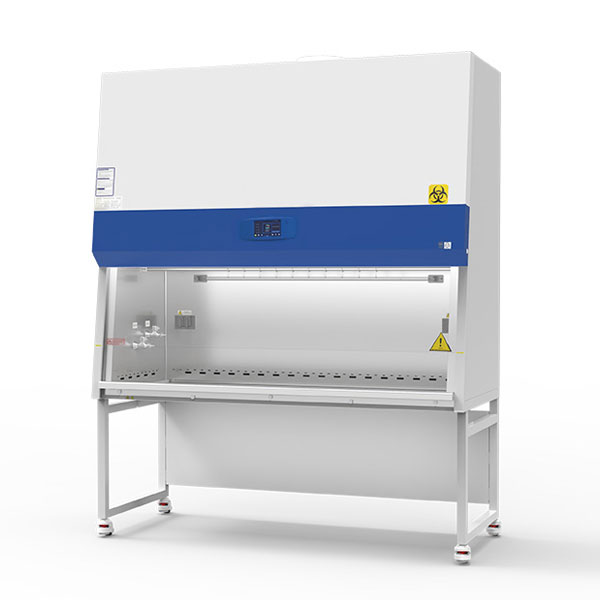
A Biosafety Cabinet (BSC), specifically a Class II type, is a primary containment device used in laboratories to provide a safe working environment for personnel, the product, and the surrounding environment. It is a ventilated, enclosed workspace designed to protect the user from exposure to biohazardous aerosols generated during procedures like pipetting, mixing, or centrifugation. Simultaneously, it protects the materials or cell cultures inside from contamination by room air, and it filters potentially contaminated air before it is exhausted back into the laboratory.
Unlike a fume hood, which only protects the user, or a laminar flow clean bench, which only protects the product, the Class II BSC offers this triple layer of protection, making it indispensable for work with infectious agents (Risk Groups 2, 3, and 4 when properly configured) and sensitive cell cultures.
How it Works
A Class II BSC operates on the principle of directional, HEPA-filtered airflow.
- Inflow: Room air is drawn into the front grille of the cabinet by an internal fan. This constant, inward airflow (typically at a minimum face velocity of 100 feet per minute) creates an “air curtain” at the front opening, acting as a barrier to prevent aerosols from escaping into the lab.
- Downflow: The fan forces a portion of this air (combined with recirculated cabinet air) through a HEPA filter in the top of the cabinet. This creates a sterile, vertical, laminar downflow of clean air that bathes the work surface, protecting the samples from contamination.
- Recirculation & Exhaust: About 70% of the downflow air is recirculated back through the supply HEPA filter. The remaining 30%, along with the inflow air captured at the front grille, is directed through dedicated channels and exhausted. In most types (like Class II, Type A2), this exhaust air is passed through another HEPA filter before being returned to the lab room or ducted outside (in the case of Class II, Type B2).
This balanced system of inflow, downflow, and exhaust ensures the triple-containment objective.
Key Components
- Cabinet Enclosure: The metal housing (typically stainless steel for durability and cleanability) that defines the workspace and airflow paths.
- Work Zone/Area: The sterile, illuminated interior space where procedures are performed.
- Front Sash: The movable glass panel that provides access. It must be kept at the certified operating height (usually marked) for proper airflow.
- HEPA Filters: High-Efficiency Particulate Air filters are the heart of the BSC. They remove 99.97% of particles 0.3 microns in diameter, trapping microorganisms and ensuring sterile downflow and clean exhaust. Both supply (for downflow) and exhaust (for outflow) filters are used.
- Blower/Fan: The motorized fan that creates the necessary pressure and volume to maintain consistent directional airflow.
- Inflow Grille: The perforated area at the front or bottom of the work opening that captures room air.
- Exhaust Grille: Located at the rear or top of the work area, it captures contaminated air for filtration and exhaust.
- Control Panel: Houses controls for the blower, lights, UV light (if equipped), and alarms.
- Alarm System: Typically monitors airflow (via a pressure sensor) and alerts the user if the face velocity falls outside safe parameters.
- UV Germicidal Lamp (Optional): Used for surface decontamination of the work zone when the cabinet is not in use. It is NOT a substitute for proper chemical disinfection and must never be used while the cabinet is occupied.
- Ducts and Plenums: The sealed internal passages that direct air to and from the filters.
2. Uses
Clinical Applications
- Microbiology & Virology: Processing of bacterial cultures, tuberculosis samples, and viruses (e.g., influenza, SARS-CoV-2, HIV).
- Cell Culture & Tissue Culture: Maintaining sterile mammalian cell lines for research, vaccine development, or regenerative medicine.
- Pharmaceutical Compounding: Aseptic preparation of intravenous admixtures, chemotherapy drugs, and other sterile medications in hospital pharmacies.
- Pathology & Histology: Handling tissue samples that may contain infectious agents.
- Diagnostic Testing: Processing of potentially infectious patient samples (sputum, blood, CSF) for PCR, serology, or culture.
- Forensic Laboratories: Handling evidence that may contain biological hazards.
Who Uses It
- Clinical Laboratory Scientists/Medical Technologists
- Microbiologists and Virologists
- Research Scientists and Post-Doctoral Fellows
- Cell Culture Technicians
- Hospital Pharmacists (for IV admixture)
- Pathology Assistants
- Public Health Laboratory Personnel
Departments/Settings
- Hospital Clinical Laboratories (Microbiology, Virology, Pathology)
- Hospital Pharmacy (IV Rooms)
- Public Health and Reference Laboratories
- University and Biotech Research Laboratories
- Pharmaceutical and Vaccine Manufacturing Facilities (R&D and QC labs)
- Blood Banks and Centers for Disease Control
3. Technical Specifications
Typical Specifications
- Face Velocity: 100-110 feet per minute (fpm) ±10% (for Type A2/B2 cabinets).
- Downflow Velocity: Varies by model but typically 50-75 fpm.
- HEPA Filtration Efficiency: 99.99% (EN1822) or 99.97% (IEST) on particles ≥0.3 µm.
- Noise Level: <65 dBA.
- Vibration: Low vibration models are available for micromanipulation work.
- Illumination: >1000 lux at the work surface.
- Electrical: Typically 115V/60Hz or 230V/50Hz, with consumption ranging from 500W to 1500W.
Variants & Sizes
- Sizes: Defined by interior work surface width. Common sizes are 2ft (0.6m), 3ft (0.9m), 4ft (1.2m), 5ft (1.5m), and 6ft (1.8m).
- Types (NSF/ANSI 49 Standard Classification):
- Type A1: Fixed opening, 75% air recirculated, exhausts into room. Less common now.
- Type A2 (Most Common): Opening height ~10 inches, 70% recirculated, 30% exhausted through a HEPA filter back into the room. Suitable for Risk Groups 1-3.
- Type B1: 40% recirculated, 60% exhausted via a dedicated duct; used for low levels of volatile toxic chemicals.
- Type B2 (Total Exhaust, “Ducted”): 0% recirculation, 100% exhausted via hard-ducting. Used for higher-risk agents and volatile chemicals. Requires specialized HVAC.
- Type C1: A hybrid that can operate as an A2 (recirculating) or B2 (ducted) cabinet, offering flexibility.
Materials & Features
- Construction: 304 or 316 grade stainless steel interior (smooth, crevice-free, easy to clean). Exterior is often powder-coated carbon steel.
- Sash: Tempered safety glass, often with a counterbalanced mechanism.
- Advanced Features: Digital display for face/downflow velocity and filter life, touch-screen controls, wireless data logging for validation, auto-sash closure, vapor-proof designs for decontamination, ergonomic armrests, and gas/service fittings.
Notable Models
- Thermo Fisher Scientific: Forma™ Series II, HERAsafe™
- ESCO: Airstream® Premium, Cytodynamic®
- NuAire: NU-440, NU-540 Class II, Type A2
- Labconco: Purifier® Logic®, Protector®
- Baker Company: SterilGARD®, BioPROTECT®
4. Benefits & Risks
Advantages
- Triple Protection: Uniquely safeguards personnel, product, and environment.
- Versatility: Applicable across a wide range of biosafety levels and applications.
- Improved Sample Integrity: HEPA-filtered downflow creates an ISO 5 (Class 100) clean environment for sensitive cultures.
- Regulatory Compliance: Essential for labs working with regulated pathogens and for compliance with standards like NIH/CDC Biosafety in Microbiological and Biomedical Laboratories (BMBL).
Limitations
- Not for Hazardous Chemicals: Most types (especially A2) are not designed for significant volumes of volatile toxic chemicals or radionuclides, which require a ducted fume hood or Type B2 cabinet.
- Requires Space & Maintenance: Needs dedicated space, regular certification, and filter changes.
- Airflow Sensitivity: Workflow, room drafts, and personnel movement can disrupt the critical air barrier if not used properly.
Safety Concerns & Warnings
- Never use an open flame (Bunsen burner) inside a modern Class II BSC. It disrupts airflow and can damage HEPA filters. Use sterile disposable loops or electric micro-incinerators instead.
- Operate at the correct sash height. This is critical for maintaining proper face velocity.
- Avoid cluttering the front and rear grilles. This can severely disrupt airflow patterns.
- Decontaminate the work surface before and after every use with an appropriate disinfectant (e.g., 70% ethanol, diluted bleach).
- Allow the cabinet to run for at least 3-5 minutes (“purge cycle”) before and after work to establish airflow and purge contaminants.
- UV lamps are a supplemental decontamination tool only and do not replace chemical disinfection.
Contraindications
A Class II BSC (especially Type A2) is contraindicated for:
- Work with large volumes of volatile toxic chemicals or radionuclides.
- Procedures that generate excessive amounts of aerosols which may overwhelm the air curtain.
- Use as a fume hood, chemical storage cabinet, or general-purpose enclosure.
5. Regulation
FDA Class
In the USA, Class II BSCs are regulated as Class II Medical Devices (Product Code: FFQ) when intended for medical purposes (e.g., compounding sterile drugs). They are subject to 510(k) premarket notification.
EU MDR Class
Under EU MDR 2017/745, BSCs are classified as Class IIb devices (Rule 12) as they are equipment intended for controlling or monitoring a physiological process. They require a conformity assessment by a Notified Body.
CDSCO Category
In India, under the Medical Device Rules, 2017, BSCs are classified as Class C (Moderate-High Risk), requiring a conformity assessment by a notified body.
PMDA Notes
In Japan, BSCs are regulated as Class II Specified Controlled Medical Devices. Marketing approval requires certification against the Japanese Industrial Standards (JIS K 3800) and compliance with Pharmaceutical and Medical Device Act (PMD Act) requirements.
ISO/IEC Standards
- NSF/ANSI 49: Biosafety Cabinetry: Design, Construction, Performance, and Field Certification. This is the primary global standard.
- EN 12469: Biotechnology – Performance criteria for microbiological safety cabinets (European standard).
- ISO 14644-1: Specifies cleanroom classifications (relevant for the downflow air quality).
- ISO/IEC 17025: General requirements for the competence of testing and calibration laboratories (relevant for field certifiers).
6. Maintenance
Cleaning & Sterilization
- Daily/Routine: Wipe all interior surfaces with a disinfectant (e.g., 70% isopropyl alcohol) before and after each work session. Wipe from clean to dirty areas.
- Weekly/Deep Clean: Turn off the cabinet. Use a milder disinfectant like a diluted bleach solution (1:10) or a phenolic compound, ensuring all surfaces, including side and rear walls, are treated. Rinse with water or 70% alcohol to prevent corrosion. Never spray liquids directly onto HEPA filters.
Reprocessing
Not applicable in the same sense as surgical instruments. The primary “reprocessing” is the surface decontamination described above.
Calibration & Certification
- Field Certification: Must be performed annually and after every move or filter change by a qualified professional.
- Tests Include: Inflow velocity, downflow velocity, HEPA filter integrity (DOP/PAO challenge test), smoke pattern test for airflow, noise, vibration, and light intensity.
- Calibration: Airflow monitors and sensors should be calibrated as per the manufacturer’s schedule, typically during annual certification.
Storage
If a BSC is to be taken out of service for storage:
- Perform a thorough decontamination (including gas decontamination with formaldehyde or vaporized hydrogen peroxide if used with high-risk agents).
- Seal openings (front sash, grilles) with plastic.
- Store in a clean, dry location. Label it as “Decontaminated.”
7. Procurement Guide
How to Select the Device
- Assess Risk: What biological agents (Risk Group) and chemicals will be used? This determines the Type (A2 vs. B2).
- Determine Size: Based on required work surface, equipment footprint (microscopes, centrifuges), and available lab space.
- Consider Ergonomics: Height, armrest comfort, sash type (vertical or horizontal), noise, and vibration.
- Evaluate Room Infrastructure: Does the lab have ducting capabilities for a Type B2? Is the electrical supply adequate?
- Plan for Validation: Ensure there is local access to qualified field certifiers.
Quality Factors
- Compliance with Standards: Must be certified to NSF/ANSI 49 or EN 12469.
- Construction Quality: Seamless stainless steel welds, no crevices, durable finish.
- Control System: User-friendly interface with clear alarms and diagnostics.
- Service & Support: Availability of manufacturer or third-party service contracts and spare parts.
Certifications
Look for the NSF Mark on the cabinet, indicating it has been listed by NSF International. Also check for CE Marking (for Europe) and other regional certifications.
Compatibility
Ensure the cabinet can accommodate any specific equipment (e.g., microscopes, pipet controllers) you plan to use inside. Check if service fittings (gas, vacuum) are needed and available.
Typical Pricing Range
Prices vary significantly by type, size, and features.
- Class II, Type A2: $5,000 – $15,000 USD
- Class II, Type B2: $15,000 – $30,000+ USD
(Excluding installation, ductwork, and certification costs.)
8. Top 10 Manufacturers (Worldwide)
- Thermo Fisher Scientific (USA) – Global life sciences leader; offers the Forma™ and HERAsafe™ lines.
- ESCO Lifesciences (Singapore) – Major innovator and volume manufacturer; Airstream® and Cytodynamic® series.
- NuAire, Inc. (USA) – Pioneers in biosafety cabinetry; known for NU-400 and NU-500 series.
- Labconco Corporation (USA) – Specializes in laboratory equipment; Purifier® and Protector® lines.
- The Baker Company (USA) – Specializes in containment equipment; SterilGARD® and BioPROTECT®.
- Heal Force Bio-meditech Holdings (China) – Major Asian manufacturer; offers a wide range of BSCs.
- Germfree Laboratories, Inc. (USA) – Known for custom and high-containment solutions.
- Kewaunee Scientific Corporation (USA) – Provides lab furniture and equipment including BSCs.
- Telstar Life Science Solutions (Spain) – Part of the Azbil Group; known for advanced engineering.
- Berner International (Germany) – Known for high-quality safety and containment equipment in Europe.
9. Top 10 Exporting Countries (Latest Year – Based on HS Code 842139 trends)
Ranked by estimated export value of “Filtering or Purifying Machinery and Apparatus for Gases” including BSCs.
- China – Dominant global supplier, offering a wide range from economical to high-end models.
- United States – Home to major innovators and manufacturers, exporting premium and specialized cabinets.
- Germany – Leading European exporter of high-precision engineering and containment technology.
- Singapore – A key hub, largely driven by ESCO’s manufacturing and global distribution.
- Italy – Significant manufacturer and exporter of laboratory equipment to Europe and beyond.
- United Kingdom – Exports specialized containment solutions and has a strong research sector.
- Japan – Exports high-tech BSCs, often with advanced monitoring and control systems.
- France – Major player in the European life sciences and pharmaceutical market.
- South Korea – Growing exporter of laboratory equipment, including BSCs, with strong R&D.
- India – Rapidly growing domestic manufacturer and exporter to emerging markets.
10. Market Trends
Current Global Trends
- Rising Demand Post-Pandemic: Increased awareness and investment in biosecurity and public health infrastructure globally.
- Growth in Pharma & Biotech: Expansion in cell/gene therapy, vaccine development, and biologics manufacturing is driving demand.
- Modular & Flexible Labs: Demand for cabinets that integrate seamlessly with modular lab furniture and facility designs.
New Technologies
- Smart Cabinets: IoT-enabled BSCs with remote monitoring, predictive maintenance alerts, and digital validation logs.
- Energy Efficiency: Variable Air Volume (VAV) controls that adjust airflow based on sash position, reducing energy consumption.
- Enhanced Ergonomics: Improved lighting, reduced noise/vibration, and ergonomic designs to reduce user fatigue.
- Advanced Materials: Antimicrobial coatings and even smoother surface finishes for easier decontamination.
Demand Drivers
- Stringent Regulatory Standards for drug compounding (USP <797>, <800>) and pathogen research.
- Increased Funding for infectious disease research and pandemic preparedness.
- Growth of the Biotechnology Industry.
- Aging Healthcare Infrastructure replacement and modernization in developed countries.
Future Insights
The market will continue to grow, with a focus on connectivity, user safety data, and sustainability. Integration with Building Management Systems (BMS) and Laboratory Information Management Systems (LIMS) will become standard. Demand in Asia-Pacific, particularly China and India, is expected to outpace other regions due to expanding healthcare and research sectors.
11. Training
Required Competency
Users must complete hands-on, practical training covering:
- Theory of airflow and containment.
- Proper work practices (material placement, slow movements).
- Decontamination procedures.
- Emergency response (power failure, spill cleanup).
- Recognition of alarm conditions.
Common User Errors
- Rapid Arm Movement: Disrupts the air barrier. Move arms in and out slowly and perpendicular to the sash.
- Overloading the Workspace: Blocks front and rear grilles, compromising airflow.
- Working at the Wrong Sash Height: The most common error. Always check the marked operating height.
- Using Incompatible Materials: Using volatile chemicals not approved for the cabinet type.
- Poor Surface Decontamination: Inconsistent or inadequate wiping, leaving contamination zones.
Best-Practice Tips
- Plan your work: Assemble all materials inside the cabinet before starting. Perform work from “clean to dirty.”
- Minimize traffic: Reduce people walking behind you while working to prevent drafts.
- Use proper PPE: Always wear a lab coat and gloves. Additional respiratory protection may be needed based on risk assessment.
- Annual Certification is Non-Negotiable: Never operate an uncertified cabinet.
12. FAQs
1. What’s the difference between a Class I, Class II, and Class III BSC?
- Class I: Protects the user and environment only (inflow HEPA-filtered exhaust). Does not protect samples.
- Class II: Protects user, sample, and environment. Has HEPA-filtered downflow and exhaust.
- Class III: Maximum containment. Gas-tight, glove box design for Risk Group 4 agents. All air is double-HEPA filtered.
2. Can I use a Bunsen burner inside my Class II BSC?
No. It disrupts the laminar airflow, creates heat turbulence, and can damage the HEPA filters. Use sterile, disposable inoculating loops or electric micro-incinerators placed at the rear of the workspace.
3. How often does my BSC need to be certified?
At least annually, and always after it has been moved or after a HEPA filter change.
4. My BSC’s alarm is sounding. What should I do?
Immediately stop work, carefully close any open containers, and slowly remove your arms. Check the digital readout (if available) and consult the manual. The most common cause is the sash being raised above the operating height. If the alarm persists, secure the cabinet and contact your lab manager or service technician.
5. How long should I run the UV light for decontamination?
UV light is a secondary tool. Effective surface decontamination typically requires 15-30 minutes of direct exposure with the sash closed. Remember: Chemical disinfection is primary. UV does not penetrate spills or shadows.
6. Can I work with hazardous chemicals in a Type A2 BSC?
Only very minute quantities of low-risk, volatile chemicals. For significant chemical use, you need a Type B2 (ducted) cabinet or a dedicated fume hood.
7. How do I properly clean a major spill inside the BSC?
- Keep the blower running.
- Pour disinfectant (e.g., bleach) from the edges of the spill toward the center.
- Cover with absorbent towels and let sit for the required contact time (e.g., 20 mins for bleach).
- Wipe up carefully, placing all waste in a biohazard bag inside the cabinet.
- Wipe the entire surface again with fresh disinfectant.
8. What is the typical lifespan of a BSC?
With proper maintenance, annual certification, and timely filter changes, a high-quality BSC can last 15-20 years or more.
13. Conclusion
The Class II Biosafety Cabinet is a cornerstone of modern biosafe laboratory practice. Its unique ability to provide triple protection makes it essential for a vast array of clinical, research, and pharmaceutical applications. Selecting the correct type (A2 vs. B2), using it with strict adherence to best practices, and maintaining it through rigorous annual certification are non-negotiable responsibilities for any laboratory. As technology advances, these cabinets are becoming smarter and more integrated, but their core function—safeguarding lives and the integrity of scientific work—remains paramount. A well-chosen, properly maintained, and correctly operated BSC is not just a piece of equipment; it is a critical component of a laboratory’s safety culture.
14. References
- Centers for Disease Control and Prevention (CDC) & National Institutes of Health (NIH). (2020). Biosafety in Microbiological and Biomedical Laboratories (BMBL), 6th Edition.
- NSF International. (2022). NSF/ANSI 49: Biosafety Cabinetry: Design, Construction, Performance, and Field Certification.
- European Committee for Standardization (CEN). (2000). EN 12469: Biotechnology – Performance criteria for microbiological safety cabinets.
- U.S. Food and Drug Administration (FDA). Code of Federal Regulations, Title 21, Part 880 – Medical Devices.
- World Health Organization (WHO). (2020). Laboratory Biosafety Manual, 4th Edition.
- Kruse, R. H., Puckett, W. H., & Richardson, J. H. (1991). Biological Safety Cabinetry. Clinical Microbiology Reviews.
- Sandia National Laboratories. Biosafety Cabinet Training Materials and Guides.
- Global Market Insights, Inc. (2023). Biosafety Cabinets Market Size Report.
- International Society for Pharmaceutical Engineering (ISPE). Baseline Guide: Sterile Product Manufacturing Facilities.
- United States Pharmacopeia (USP). General Chapters <797> Pharmaceutical Compounding – Sterile Preparations and <800> Hazardous Drugs.