1. Definition
What is an Otoscope?
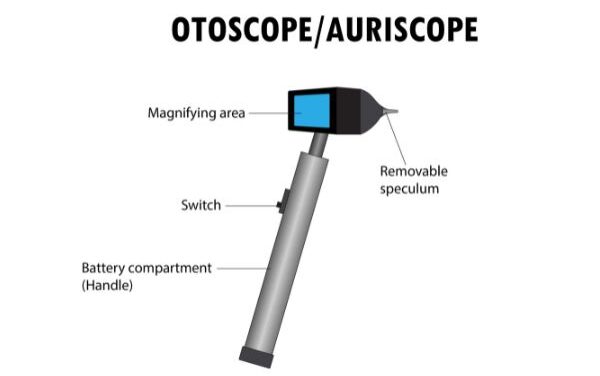
An otoscope, also known as an auriscope, is a handheld, portable medical device primarily used for examining the external auditory canal (the ear canal) and the tympanic membrane (the eardrum). Its primary function is to provide a well-lit, magnified view of these structures, enabling healthcare providers to assess ear health, diagnose infections, check for blockages, and perform minor procedures. It is one of the most fundamental and frequently used tools in physical examination.
How it Works
The otoscope works on a simple optical principle. A bright light source (traditionally a halogen bulb, now often an LED) is projected through a disposable speculum (a cone-shaped tip) inserted into the ear canal. This illuminates the dark cavity. The clinician looks through a viewing lens (with low-level magnification, typically 3x to 8x) on the opposite side. The light reflects off the eardrum and canal walls, and this image is transmitted through an optical system (a series of lenses or a fiber-optic bundle) to the viewer’s eye, providing a clear, enlarged view.
Key Components
- Head/Handle: Contains the power source (batteries). It is the main body held by the user.
- Light Source: An LED or halogen bulb that provides bright, cool, white illumination.
- Magnifying Lens: A viewing window with low-power magnification to enlarge the examined area.
- Speculum: A disposable, cone-shaped tip made of plastic that is inserted into the ear canal. It comes in various sizes (typically 2mm to 10mm) to fit patients of all ages.
- Lens Cap/Window: A clear cover that protects the internal optics and can be removed for cleaning.
- Insufflator Port: A nipple or port on some otoscope heads where a rubber bulb can be attached. Squeezing this bulb gently pumps air into the canal to assess eardrum mobility (pneumatic otoscopy), a key test for detecting middle ear fluid.
2. Uses
Clinical Applications
- Diagnosis of Otitis Media & Externa: Identifying signs of middle ear infection (redness, bulging, fluid behind the eardrum) or outer ear infection (swelling, discharge, canal inflammation).
- Cerumen (Earwax) Management: Visualizing and, with specialized attachments, aiding in the removal of earwax impaction.
- Foreign Body Removal: Locating and assisting in the extraction of objects lodged in the ear canal.
- Tympanic Membrane Assessment: Evaluating the eardrum for perforations (holes), scarring (tympanosclerosis), retraction, or signs of cholesteatoma.
- Trauma Evaluation: Assessing the ear for injuries from cotton swabs, pressure changes (barotrauma), or blunt force.
- Screening & Routine Examinations: A standard part of well-child checkups, pre-employment physicals, and annual exams.
- Surgical Procedures: Used in minor office procedures like tympanostomy tube placement or biopsies.
Who Uses It
- Primary Care Physicians (Family Medicine, Pediatricians)
- Otolaryngologists (ENT Specialists)
- Emergency Room Doctors and Nurses
- Urgent Care Practitioners
- Audiologists
- School Nurses
- Advanced Practice Providers (Nurse Practitioners, Physician Assistants)
Departments/Settings
- Outpatient Clinics (Primary Care, Pediatrics, ENT)
- Hospital Emergency Departments
- Inpatient Hospital Wards
- Urgent Care Centers
- Audiology and Hearing Aid Centers
- School and University Health Services
3. Technical Specs
Typical Specifications
- Magnification: 3x to 8x
- Light Source: LED (most common, 3,000-6,000K color temperature) or Halogen bulb.
- Power Source: Typically AA or rechargeable batteries (3.7V Li-ion).
- Viewing Angle: Fixed straight (0°) or diagnostic (wide-angle, typically 10°-25°).
- Illumination: LED lifespan ~50,000 hours.
Variants & Sizes
- Pocket/Full-Size: Traditional design with a reusable handle and interchangeable head.
- Pocket LED Penlights: Ultra-compact, all-in-one units.
- Video/Digital Otoscopes: Feature a camera and display screen (on device or connected to a monitor/PC) for recording, sharing, and enhanced visualization.
- Welch Allyn MacroView: A popular variant with a significantly larger lens and wider field of view, providing an “immediate panoramic view” of the entire eardrum.
Materials & Features
- Materials: Durable medical-grade plastics and stainless steel. Specula are single-use plastic.
- Features: Pneumatic capability (insufflator port), fiber-optic illumination (prevents heat transfer), focus wheels (on some models), smartphone/tablet connectivity (for digital models).
Models
- Welch Allyn MacroView: Industry standard for high-quality traditional otoscopy.
- Heine Mini 3000: Renowned German-engineered, modular design.
- Riester ri-scope: Popular high-quality, cost-effective option.
- Firefly DE500/Finhoff FF520: Common rechargeable, all-in-one LED otoscopes.
- CellScope Oto: Smartphone-connected digital otoscope for telemedicine.
4. Benefits & Risks
Advantages
- Non-invasive & Rapid: Provides immediate diagnostic information without complex procedures.
- Portable & Versatile: Essential for bedside, clinic, and field examinations.
- Improves Diagnostic Accuracy: Enables direct visualization, leading to better diagnosis of common conditions like ear infections.
- Cost-Effective: The device itself is relatively inexpensive, and disposable specula prevent cross-contamination.
- Patient Education: Digital/video models allow patients to see their own eardrum, improving understanding and compliance.
Limitations
- User-Dependent: Image quality and diagnostic accuracy heavily rely on the skill of the examiner.
- Limited View: Only visualizes the outer ear canal and eardrum surface; cannot see the middle or inner ear structures directly.
- Obstruction: View can be blocked by cerumen, discharge, or canal swelling.
Safety Concerns & Warnings
- Speculum Size: Using too large a speculum can cause pain or injury to the ear canal.
- Insertion Depth: Never force the otoscope. Insert only as far as needed to see the eardrum, typically 1-2 cm in adults.
- Patient Movement: Sudden movement by the patient (especially children) can lead to canal abrasion or perforation. Proper head stabilization is crucial.
- Infection Control: Always use a new, disposable speculum for each patient. Clean the otoscope head between patients per protocol.
Contraindications
- Absolute: Suspected or confirmed acute trauma with cerebrospinal fluid leak (CSF otorrhea).
- Relative/Caution: Severe otitis externa with extreme swelling/pain, recent ear surgery (consult surgeon first), an uncooperative patient where restraint may cause harm.
5. Regulation
Otoscopes are generally considered low to moderate-risk devices.
- FDA Class: Most are Class I (exempt from premarket notification). Otoscopes with pneumatic capability or specialized surgical attachments may be Class II.
- EU MDR Class: Typically Class I (non-sterile, non-measuring). If intended for monitoring vital physiological processes (e.g., specific surgical monitoring), they could be Class IIa.
- CDSCO Category: Class A (low risk) under India’s Medical Device Rules.
- PMDA Notes: In Japan, they are classified as Class I “General Medical Devices.”
- ISO/IEC Standards:
- ISO 10993-1: Biological evaluation of medical devices.
- ISO 13485: Quality management systems for medical devices.
- IEC 60601-1: General safety requirements for medical electrical equipment.
6. Maintenance
Cleaning & Sterilization
- Between Patients: Wipe the entire otoscope head (except lens) with a hospital-grade disinfectant wipe (e.g., CaviWipe, Clorox Healthcare). Do not immerse.
- Lens Cleaning: Use a soft, lint-free cloth with lens cleaner. Avoid abrasive materials.
- Handle: Wipe with a disinfectant cloth.
- Sterilization: Otoscope heads are generally not sterilizable unless specified by the manufacturer (some autoclaveable ENT heads exist).
Reprocessing
For reusable, non-disposable parts: Clean → Disinfect → Air Dry → Store. The speculum is single-use only.
Calibration
Optical otoscopes do not require electronic calibration. Regular checks for light brightness and clarity, lens integrity, and pneumatic bulb function (if equipped) are recommended.
Storage
Store in a clean, dry place at room temperature. Remove batteries if not used for extended periods to prevent corrosion. Keep a full range of speculum sizes available.
7. Procurement Guide
How to Select the Device
Consider: Primary user (ENT vs. pediatrician), setting (clinic vs. ER), need for pneumatic function, preference for traditional vs. wide-view optics, and budget.
Quality Factors
- Optical Clarity: Sharp, bright, distortion-free view.
- Build Quality: Durable materials, secure battery compartment.
- Illumination: Bright, white, even light with no hot spots.
- Ergonomics: Comfortable grip, easy one-handed operation.
- Brand Reputation & Service: Reliable manufacturer with good warranty and support.
Certifications
Look for CE Marking (EU), FDA Cleared/Registered (US), and possibly ISO 13485 certification of the manufacturer.
Compatibility
Ensure specula are universally compatible or readily available for the chosen model. For digital systems, check software compatibility with your existing health record systems.
Typical Pricing Range
- Traditional Pocket Otoscope: $150 – $400
- High-End Diagnostic (MacroView) Set: $500 – $1,200
- Basic Pocket LED Penlight: $50 – $150
- Consumer/Prosumer Digital Otoscope: $200 – $500
- Professional Clinical Digital Otoscope System: $1,500 – $4,000+
8. Top 10 Manufacturers (Worldwide)
- Hill-Rom (Welch Allyn) – USA: The market leader. Renowned for the Welch Allyn brand, particularly their MacroView otoscope. Known for exceptional quality and durability.
- Heine – Germany: Premium manufacturer of precision optical instruments. The Heine Mini 3000 series is a gold standard for modular otoscopes.
- Riester – Germany: Family-owned company producing high-quality, ergonomic diagnostic equipment like the ri-scope.
- American Diagnostic Corporation (ADC) – USA: Offers a wide range of reliable and cost-effective diagnostic tools, including otoscopes.
- Medline – USA: Global manufacturer and distributor providing a variety of medical supplies, including otoscope kits for different care settings.
- Rudolf Riester GmbH (part of Halma) – Germany: (Note: Often listed separately from Riester) Known for robust designs.
- Keeler (Halma) – UK/USA: Specializes in optical and ophthalmic instruments, offering high-end otoscopes often preferred by ENTs.
- Inventis – Italy: Focus on audiology and ENT instruments, producing otoscopes with excellent optics.
- Mabis Healthcare – USA: (Now part of McKesson) Provides affordable and reliable healthcare products, including basic otoscope sets.
- Gowllands Medical Devices – UK: Manufacturer of a range of medical devices, including otoscopes distributed under various brands.
9. Top 10 Exporting Countries (Latest Year)
(Based on harmonized trade code 901890 for “Instruments used in medical sciences”)
- United States: Dominant exporter, home to major players like Welch Allyn. High-value, technologically advanced devices.
- Germany: Exports premium, precision-engineered instruments from Heine, Riester, etc.
- China: Major volume exporter of cost-effective and OEM devices, increasingly improving quality.
- Japan: Exports high-quality electronic and optical medical devices.
- Mexico: A significant manufacturing hub for the North American market, exporting to the US and beyond.
- United Kingdom: Exports specialized diagnostic equipment.
- France: Home to several medical technology firms.
- Netherlands: Major European logistics and trade hub for medical devices.
- Ireland: Hosts manufacturing plants for many multinational med-tech corporations.
- Switzerland: Exports high-precision, niche medical instruments.
10. Market Trends
- Current Global Trends: Shift from halogen to LED illumination (brighter, cooler, longer-lasting). Growth of telemedicine is driving demand for digital/video otoscopes. Increasing focus on ergonomics and infection prevention.
- New Technologies: AI-assisted diagnosis software that can analyze otoscopic images to suggest pathologies. Smartphone integration for point-of-care documentation and remote consultation.
- Demand Drivers: Rising global prevalence of ear infections (especially in pediatrics), increasing ENT surgical volumes, expansion of primary care infrastructure in developing nations, and aging population with hearing-related issues.
- Future Insights: The otoscope will evolve from a simple visual tool to a connected diagnostic node. Expect more widespread use of AI, 3D imaging, and integration with electronic health records for seamless data capture and analysis.
11. Training
Required Competency
Basic competency includes: understanding ear anatomy, proper patient positioning (pull pinna up and back for adults, down and back for children), correct otoscope grip (pencil grip against the patient’s head), systematic visualization of the canal and all quadrants of the eardrum, and interpretation of common findings.
Common User Errors
- Using the Wrong Speculum Size: Causing discomfort or missing pathology.
- Improper Grip: Holding the otoscope rigidly, risking injury if the patient moves.
- Obscuring the View: Failing to clear cerumen from the canal first.
- Rushing the Exam: Not methodically inspecting the entire tympanic membrane.
- Misinterpreting Redness: A red eardrum can be from crying or fever, not just infection.
Best-Practice Tips
- Always use a disposable speculum.
- Stabilize: Brace your hand holding the otoscope against the patient’s head.
- Gentle Traction: Use your other hand to position the pinna optimally.
- Look Before You Insert: Briefly inspect the outer ear for abnormalities.
- Systematic Scan: Identify key landmarks (handle of malleus, light reflex, pars tensa/flaccida).
- Pneumatic Otoscopy: Learn and use it to assess eardrum mobility—it dramatically improves diagnostic accuracy for otitis media.
12. FAQs
Q1: How often should I replace the otoscope bulb?
A: With modern LEDs, almost never during the device’s lifespan. For halogen bulbs, replace them when they burn out or if the light becomes dim/yellow.
Q2: Can I clean and reuse a plastic speculum?
A: No. Plastic specula are designed for single-use only to prevent cross-contamination and infection. They are not designed to be effectively sterilized.
Q3: What’s the difference between a 3.5v and a 3.7v otoscope?
A: The voltage relates to the power system. A 3.7v model typically uses a brighter LED and a rechargeable lithium battery. A 3.5v model often uses standard AA batteries and may have a halogen bulb. Brightness and battery life are the key practical differences.
Q4: My view is always blurry. What’s wrong?
A: The lens on the otoscope head is likely dirty. Gently clean it with a lens cloth. Also, ensure the speculum is fully and securely attached.
Q5: Why can’t I see the eardrum?
A: The most common reason is cerumen (earwax) obstruction. The ear canal may need to be cleaned first. Other reasons include swelling, a foreign body, or an unusually narrow or tortuous canal.
Q6: Is a more expensive otoscope worth it?
A: For frequent clinical use, yes. Higher-end models provide superior optics, brighter and truer-color illumination, better durability, and often a wider field of view (like MacroView), which makes exams easier and more accurate.
Q7: Can I use an otoscope on myself?
A: It is strongly discouraged. Self-examination is difficult, unsafe (risk of perforation), and you lack the training to interpret findings correctly. See a professional.
Q8: What does a normal eardrum look like?
A: It is pearly gray, translucent, and slightly concave. You should see the bony landmarks, notably the handle of the malleus, and a cone of light反射 in the anterior-inferior quadrant.
Q9: What is pneumatic otoscopy and why is it important?
A: It involves gently puffing air into the canal to see if the eardrum moves. A healthy eardrum is mobile. Lack of movement indicates fluid or pressure behind it (effusion), a key sign of otitis media.
Q10: Are video otoscopes good for diagnosis?
A: Yes, they offer excellent visualization on a screen, allow for image/video capture for records or consultation, and are fantastic for patient education. They are becoming a standard of care in many ENT settings.
13. Conclusion
The otoscope remains an indispensable, foundational tool in medical diagnostics. From the traditional pocket device to advanced digital systems, its core purpose is to illuminate and reveal the health of the outer ear and eardrum. Mastery of its use—through proper technique, understanding of anatomy, and systematic examination—is a fundamental clinical skill. As technology evolves, the otoscope is transitioning from a simple viewing tool to an integrated diagnostic platform, enhancing accuracy, documentation, and patient care. Selecting the right device, maintaining it properly, and adhering to best practices in its use are all critical to leveraging this simple yet powerful instrument to its fullest potential.
14. References
- American Academy of Family Physicians. (2023). Otoscopy Techniques.
- American Academy of Otolaryngology–Head and Neck Surgery. (2022). Clinical Practice Guidelines: Otitis Media with Effusion.
- Pichichero, M. E. (2020). Otitis Media. Pediatrics in Review.
- U.S. Food and Drug Administration (FDA). (2023). Device Classification Database.
- European Commission. (2023). Medical Device Regulation (MDR).
- International Organization for Standardization (ISO). ISO 13485:2016 Medical devices.
- Welch Allyn. (2023). MacroView Otoscope User Manual.
- Grand View Research. (2023). Otoscopes Market Size, Share & Trends Analysis Report.
- Tidy, C. (2022). Examination of the Ear. Patient UK Professional Reference.
- Jacobs, J. (2021). Handbook of Otoscopy. Springer.