1. Definition
What is a Suction-Irrigation Laparoscopic Probe?
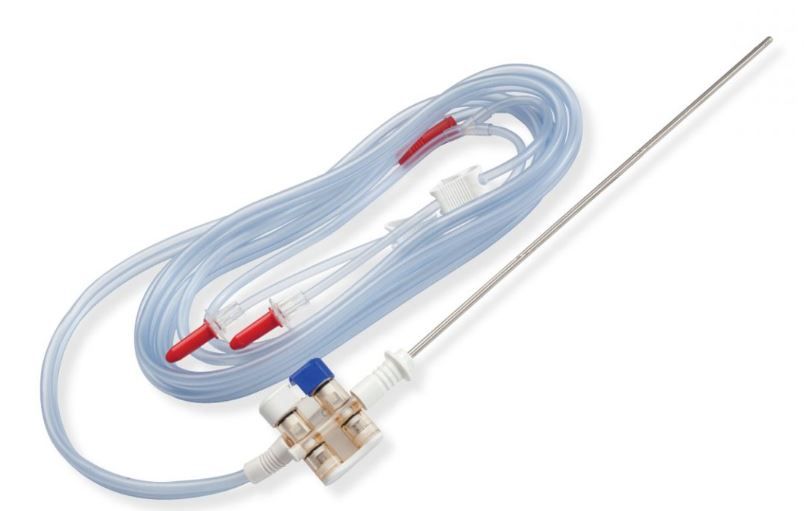
A suction-irrigation laparoscopic probe (often called an “aqua-dissector,” “irrigator-aspirator,” or simply “sucker”) is a fundamental and indispensable instrument in minimally invasive surgery (MIS). It is a long, narrow, pencil-like device that is inserted into the abdominal cavity through a small keyhole incision (typically 5-12 mm). Its primary function is dual-purpose: to deliver a controlled stream of sterile fluid (irrigation) and to remove fluids, blood, and surgical debris (suction) from the surgical field.
In essence, it acts as the surgeon’s “water hose and vacuum cleaner” inside the body, allowing them to maintain a clear view and a clean operative site without having to convert to an open procedure.
How it Works
The probe is connected via tubing to two separate external systems:
- Irrigation System: A pressurized bag or pump containing sterile saline or another irrigation solution.
- Suction System: The hospital’s central wall suction or a portable suction unit.
The probe features controls, usually a roller-wheel or trumpet valves, on its handle. The surgeon operates these controls with their fingers to independently or simultaneously activate the irrigation and suction functions. By toggling between the two, the surgeon can wash away blood to visualize a bleeding vessel, aspirate smoke from electrocautery, or clear away irrigation fluid to inspect an organ.
Key Components
- Handle: The ergonomic grip held by the surgeon. It houses the control mechanisms.
- Shaft: A long, rigid, or sometimes flexible, tubular stem that traverses the trocar (port) into the body cavity. It is typically made of stainless steel for durability and reusability.
- Tip/Nozzle: The distal end of the shaft where fluid is expelled and suction is applied. Tip designs vary (e.g., rounded, multi-hole, angled) for different surgical tasks.
- Control Valves: Mechanisms on the handle to regulate flow. A common type is a dual trumpet valve—one for suction, one for irrigation. Another is a single roller-wheel that toggles between the two functions.
- Irrigation Port: A Luer-lock or barbed connector on the handle for attaching the irrigation tubing.
- Suction Port: A larger connector for attaching the suction tubing to the wall suction unit.
2. Uses
Clinical Applications
The suction-irrigation probe is used across a vast spectrum of laparoscopic procedures, including but not limited to:
- Laparoscopic Cholecystectomy (Gallbladder Removal): To irrigate the liver bed and suction out bile or blood.
- Gynecological Surgeries (Hysterectomy, Cyst Removal): To irrigate the pelvic cavity, remove old blood (e.g., in ectopic pregnancy), and maintain visualization.
- Bariatric Surgery: To clean and expose tissues during gastric bypass or sleeve gastrectomy.
- Colorectal Surgery: To lavage the abdominal cavity in cases of perforation or infection and suction out fecal contaminants.
- Appendectomy: To irrigate the right lower quadrant after removal of an inflamed appendix.
- Hernia Repair: To clear the pre-peritoneal space and provide a dry field for mesh placement.
- Diagnostic Laparoscopy: To wash the peritoneal cavity for cytological analysis in oncology.
Who Uses It
- Laparoscopic Surgeons: The primary users, across specialties like General Surgery, Gynecology, and Urology.
- Surgical Assistants: Often manage the probe under the surgeon’s direction to aid in exposure.
- Scrub Nurses/Technologists: Responsible for preparing, testing, and handing the probe to the surgeon and for managing the external tubing connections.
Departments/Settings
- Operating Rooms (ORs) in hospitals and ambulatory surgery centers.
- Specialized Laparoscopy Suites.
- Occasionally in emergency trauma bays for rapid diagnostic laparoscopy.
3. Technical Specs
Typical Specifications
- Shaft Length: 25 cm to 35 cm (adult); 15 cm to 20 cm (pediatric).
- Shaft Diameter: 3 mm to 10 mm, with 5 mm and 10 mm being the most common.
- Suction Pressure: Operates on standard wall suction (typically up to 500 mmHg).
- Irrigation Pressure: Can be regulated from gravity feed (~50 mmHg) to pressurized bags or pumps (up to 300 mmHg).
Variants & Sizes
- By Diameter: 5mm (for smaller ports, less flow), 10mm (for higher flow and more efficient suction of clots).
- By Tip Design:
- Single-hole: For precise, high-pressure irrigation.
- Multi-hole (Showerhead): For broad, gentle lavage.
- Angled Tips: For reaching difficult anatomical areas.
- Reusable vs. Single-Use: Reusable probes are made of durable steel; single-use (disposable) probes are made of plastic and guarantee sterility and sharpness.
Materials & Features
- Materials: Stainless steel (reusable), medical-grade plastics (disposable), silicone seals.
- Features:
- Electrocautery Compatibility: Many probes have an insulated sheath, allowing them to be used with an electrocautery pencil for dissection and coagulation without needing an additional port.
- Rotating Shaft: Allows the tip to be oriented without twisting the entire instrument.
- Ergonomic Handle: Reduces surgeon hand fatigue during long procedures.
Notable Models
- Stryker: “Revolve” and “Quantum” series.
- Medtronic: “Valleylab” irrigators.
- Johnson & Johnson (Ethicon): Various models integrated with their energy devices.
- Karl Storz: A wide range of reusable and single-use models.
- Olympus: Single-use irrigation and aspiration probes.
4. Benefits & Risks
Advantages
- Enhanced Visualization: The single most critical benefit. It clears the field of blood, smoke, and debris, preventing surgical errors.
- Improved Efficiency: Combines two essential functions into one instrument, reducing instrument exchange and saving operative time.
- Therapeutic Application: Can be used for hydro-dissection (using fluid pressure to separate tissue planes) and for lavage to reduce infection risk.
- Minimally Invasive: Supports the core principle of laparoscopic surgery, leading to less patient trauma, reduced pain, and faster recovery.
Limitations
- Clogging: The small internal lumen can be clogged by large tissue fragments or thick clots.
- Limited Suction Power: Compared to open surgery suckers, the suction power is lower due to the smaller diameter.
- Thermal Loss: Irrigation with room-temperature fluid can contribute to patient hypothermia.
Safety Concerns & Warnings
- Tissue Trauma: Aggressive suction can injure delicate tissues like the bowel or liver.
- Over-irrigation: Excessive fluid can obscure the view initially and lead to fluid overload or electrolyte imbalance if absorbed in large quantities.
- Electrical Hazard: If using an electrocautery-compatible probe, insulation failure can cause stray energy burns to unintended tissues.
- Contamination: Improper sterilization can lead to cross-contamination between patients.
Contraindications
There are no direct patient contraindications for the device itself. Its use is contraindicated by the surgeon’s lack of training in its proper application. The decision to use laparoscopy (and thus the probe) may be contraindicated in patients with certain conditions like severe coagulopathy or dense adhesions.
5. Regulation
FDA Class
In the United States, suction-irrigation probes are typically classified as Class I or Class II medical devices, depending on their features. A basic probe is often Class I (exempt from premarket notification). If it is integrated with an energy device for electrocautery, it is typically Class II (requiring a 510(k) premarket notification).
EU MDR Class
Under the European Union Medical Device Regulation (EU MDR), these devices are generally classified as Class I if reusable, or Class IIa if they have a measuring function or are used for administering energy. The shift to MDR has placed greater emphasis on technical documentation and clinical evaluation.
CDSCO Category
In India, under the Central Drugs Standard Control Organization, suction-irrigation probes fall under Class B (moderate-low risk) medical devices.
PMDA Notes
In Japan, the Pharmaceuticals and Medical Devices Agency (PMDA) typically classifies these devices as Class II. They require certification from a Registered Certified Body (RCB) and must comply with Japanese Pharmaceutical and Medical Device Law (PMDL).
ISO/IEC Standards
- ISO 13485:2016: Quality Management Systems for Medical Devices.
- ISO 15223-1:2021: Symbols used on labels and documentation.
- IEC 60601-1: General safety standards for medical electrical equipment (if electrified).
- ISO 17664:2017: Processing information for reprocessing.
6. Maintenance
Cleaning & Sterilization (for Reusable Probes)
- Point-of-Use Pre-Cleaning: Flush the irrigation and suction channels immediately after use to prevent bio-material from drying inside.
- Manual Cleaning: Disassemble if possible. Brush all lumens with an enzymatic detergent. Clean the exterior.
- Automated Washer-Disinfector: Use validated cycles for laparoscopic instruments.
- Sterilization: Steam sterilization (autoclaving) is the gold standard. Low-temperature sterilization (e.g., Hydrogen Peroxide Plasma) can be used for heat-sensitive components.
Reprocessing
Strict adherence to the manufacturer’s Instructions for Use (IFU) for reprocessing is critical to prevent Hospital-Acquired Infections (HAIs). Single-use probes eliminate this burden but generate medical waste.
Calibration
Reusable probes do not typically require formal calibration. However, they should be inspected before each procedure for:
- Insulation Integrity: Using an insulation tester for electrocautery models.
- Patency: Ensuring channels are not blocked.
- Mechanical Function: Valves should operate smoothly, and the shaft should not be bent.
Storage
- Store in a clean, dry, and temperature-controlled environment.
- Protect the tip from damage. Hang if possible or store in dedicated trays.
- Ensure the device is completely dry before storage to prevent corrosion.
7. Procurement Guide
How to Select the Device
- Procedure Volume: High-volume centers may benefit from the long-term cost of reusables; low-volume centers may prefer the convenience of disposables.
- Surgeon Preference: Ergonomics and “feel” are highly subjective; involve the end-users in trials.
- Compatibility: Ensure the probe’s diameter fits your existing trocars and that any electrocautery models are compatible with your generator.
Quality Factors
- Durability: For reusables, check the warranty and expected lifecycle.
- Flow Rate: Compare irrigation and suction performance across models.
- Ease of Reprocessing: How easy is it to disassemble and clean?
- Clog Resistance: Tips designed to resist clogging can improve surgical workflow.
Certifications
Look for CE Marking (for Europe), FDA Clearance/Approval (for USA), and other regional regulatory marks to ensure quality and safety.
Compatibility
Confirm compatibility with your hospital’s suction system, irrigation pumps, and electrosurgical units.
Typical Pricing Range
- Reusable Probe: $500 – $2,000 USD (initial investment).
- Single-Use/Disposable Probe: $50 – $250 USD per unit.
8. Top 10 Manufacturers (Worldwide)
- Medtronic plc (Ireland) – A global leader in medical technology. Notable for the “Valleylab” brand of fluid management systems and compatible probes.
- Johnson & Johnson (Ethicon Inc.) (USA) – A powerhouse in surgical devices. Offers a comprehensive portfolio of laparoscopic instruments, including advanced suction-irrigation systems.
- Stryker Corporation (USA) – Known for its strong presence in orthopedics and endoscopy. The “Revolve” and “Quantum” models are widely used.
- Karl Storz SE & Co. KG (Germany) – Renowned for high-quality, durable endoscopic instruments, including a wide range of reusable and single-use probes.
- Olympus Corporation (Japan) – A leader in endoscopy, offering a range of single-use and reusable suction-irrigation devices.
- B. Braun Melsungen AG (Germany) – A major player with a broad portfolio of surgical instruments and fluid management systems.
- CONMED Corporation (USA) – Specializes in surgical devices, including a variety of laparoscopic hand instruments and suction-irrigation products.
- Richard Wolf GmbH (Germany) – A well-respected manufacturer of endoscopic equipment, known for its robust and innovative designs.
- Becton, Dickinson and Company (BD) (USA) – Offers surgical instrumentation, including laparoscopic products acquired through various mergers.
- Applied Medical Resources Corporation (USA) – Known for its innovative and cost-effective single-use laparoscopic devices, including the “GelPort” system and associated instruments.
9. Top 10 Exporting Countries (Latest Year)
(Based on analysis of trade data for HS Code 901890 – Instruments and appliances used in medical sciences)
- United States: A dominant exporter of high-value, technologically advanced medical devices.
- Germany: Renowned for precision engineering and high-quality surgical instruments.
- Ireland: A major hub for medtech manufacturing and exports, home to several top companies.
- Japan: A leader in technological innovation and high-quality electronics integrated into medical devices.
- Mexico: A key manufacturing location for many US-based companies, exporting to North and South America.
- China: A growing force, increasingly exporting mid-range and high-volume medical devices.
- Switzerland: Known for niche, high-precision surgical instruments.
- France: Home to several established medical technology firms.
- United Kingdom: Maintains a strong medtech sector post-Brexit.
- Netherlands: A key European logistics and distribution hub.
10. Market Trends
Current Global Trends
- Shift to Single-Use Devices: Driven by concerns over HAIs, the high cost of reprocessing, and supply chain reliability. This is the most significant trend.
- Integration with Energy Platforms: Probes are increasingly being designed to work seamlessly with advanced energy devices (vessel sealing, bipolar, ultrasonic).
- Value-Based Procurement: Hospitals are focusing on Total Cost of Ownership (TCO) rather than just upfront price, factoring in reprocessing costs and OR time savings.
New Technologies
- Pulsed Irrigation: Systems that deliver fluid in short, powerful bursts for more effective lavage and hydro-dissection.
- Smart Probes: Integration of sensors to monitor fluid pressure and temperature in real-time.
- Improved Ergonomics: Focus on designs that reduce surgeon fatigue and the risk of Repetitive Strain Injury (RSI).
Demand Drivers
- Rising Volume of Minimally Invasive Surgeries.
- Growing Geriatric Population requiring more surgical interventions.
- Increasing Healthcare Awareness in emerging economies.
- Stringent Sterilization Standards favoring single-use options.
Future Insights
The suction-irrigation probe will continue to be a staple of the OR. Future iterations will likely become more modular, “smarter” with feedback systems, and part of larger digital surgery ecosystems that track fluid usage and surgical workflow.
11. Training
Required Competency
- Theoretical Knowledge: Understanding the device’s components, functions, and potential hazards.
- Psychomotor Skills: Developing the hand-eye coordination to manipulate the probe in a 3D space viewed on a 2D screen, including triangulation.
- Task Training: Practicing specific tasks like controlled irrigation, suction of simulated blood, and hydro-dissection on laparoscopic box trainers or virtual reality simulators.
Common User Errors
- “Whack-a-Mole” Suction: Indiscriminate, rapid plunging of the probe in and out of the field, which is inefficient and can cause tissue trauma.
- Over-irrigation: Flooding the field and losing visualization.
- Improper Port Placement: Placing the trocar for the probe in an ergonomically poor position, leading to awkward handling.
- Failure to Pre-Clear the Tip: Placing a clogged tip into the field, wasting time.
Best-Practice Tips
- Use Intermittent Suction: Short, controlled bursts are more effective and safer than continuous suction.
- Irrigate to Identify Bleeders: A gentle stream can help locate the exact source of bleeding.
- Keep the Tip in View: Always know where your instrument is to avoid injuring unseen structures.
- Test the Device: Always test irrigation and suction outside the patient before insertion.
12. FAQs
1. Can a suction-irrigation probe be used for dissection?
Yes, through a technique called hydro-dissection. A precise jet of fluid can be used to gently separate delicate tissue planes, such as around the cystic duct or in adhesiolysis.
2. What is the difference between a 5mm and a 10mm probe?
The 10mm probe has a larger internal lumen, allowing for a higher flow rate of both irrigation and suction. It is more effective at quickly evacuating large amounts of fluid or clots.
3. Why does my suction keep getting clogged?
This is often due to attempting to aspirate large pieces of tissue or thick clots. Using a probe with a multi-hole or anti-clog tip design can help. Sometimes, briefly activating irrigation can clear the obstruction.
4. Is it safe to use a reusable probe?
Yes, provided it is reprocessed according to the manufacturer’s strict IFU and its insulation is tested before every use (if it’s an electrocautery model). The risk is in improper reprocessing.
5. How do I choose between disposable and reusable?
Consider procedure volume, reprocessing costs and capabilities, initial budget, and surgeon preference. Disposables offer guaranteed sterility and no repair costs; reusables have a lower per-use cost over time but higher upfront and maintenance costs.
6. What fluid is typically used for irrigation?
Warm, sterile normal saline (0.9% Sodium Chloride) is the most common. Lactated Ringer’s is also used. The fluid is often warmed to prevent patient hypothermia.
7. My hospital’s suction doesn’t seem strong enough for the probe. Why?
The small diameter of the probe’s lumen inherently creates resistance. Ensure your wall suction is set to an adequate pressure (often 400-500 mmHg for laparoscopy) and check all connections for leaks.
8. Can the probe be used in robotic surgery?
Yes, there are specific suction-irrigation probes designed as accessories for robotic surgical systems like the da Vinci. These are controlled by the surgeon from the console.
13. Conclusion
The suction-irrigation laparoscopic probe is a deceptively simple yet profoundly critical instrument in the armamentarium of modern surgery. Its dual functionality as a cleaner and a dissector makes it indispensable for maintaining the clear visual field upon which safe and efficient minimally invasive surgery depends. Understanding its components, applications, proper maintenance, and the evolving market landscape is essential for surgeons, OR staff, and hospital procurement teams. As technology advances, this fundamental tool will continue to integrate smarter features, but its core purpose—to see clearly and act precisely—will remain unchanged.
14. References
- U.S. Food and Drug Administration (FDA). (2023). Classify Your Medical Device.
- European Commission. (2023). Medical Device Regulation (MDR).
- International Organization for Standardization (ISO). (2016). ISO 13485:2016 Medical devices — Quality management systems.
- Fullerton, J. K., & Fuchshuber, P. (2019). The SAGES Manual of Laparoscopic Surgery. Springer.
- MedTech Europe. (2023). The European Medical Technology Industry in Figures.
- Grand View Research. (2023). Laparoscopic Devices Market Size, Share & Trends Analysis Report.
- Manufacturer Websites and Instructions for Use (IFUs) from Stryker, Medtronic, Johnson & Johnson Ethicon, and Karl Storz.