What is Dry Skind?

Dry skin, medically known as xeroderma or xerosis, occurs when the skin lacks sufficient moisture to maintain a soft and supple texture. It often manifests as rough patches that can flake or appear scaly, and in severe cases, it may crack and bleed. Dry skin can affect any part of the body but commonly impacts the hands, arms, and legs. Factors contributing to dry skin include natural predisposition, environmental conditions, and excessive hand-washing or sanitizer use.
To alleviate dry skin, lifestyle changes, and over-the-counter moisturizers are often effective. However, if symptoms persist, consultation with a dermatologist is advisable. The skin requires water and natural oils to stay healthy, functioning as the body’s primary defense against harmful microorganisms and environmental factors. Frequent hand-washing and exposure to cold, dry air, particularly in winter, can exacerbate dry skin. Overall, maintaining proper skin hydration through moisturizing and addressing underlying causes is crucial for preventing and managing dry skin.
How many Types of dry skin?

- Contact Dermatitis:
- Occurs due to irritant or allergic reactions from substances like nickel, cosmetics, detergents, or medications.
- Symptoms include dry, itchy, and red skin, often accompanied by a rash.
- Two types: Irritant contact dermatitis (exposure to irritating chemicals) and allergic contact dermatitis (exposure to allergens).
- Eczema (Atopic Dermatitis):
- Group of skin conditions leading to red, dry, bumpy, and itchy patches.
- Severe cases can cause skin cracking, increasing susceptibility to infection.
- Aggravated by irritants, allergens, and stress.
- Seborrheic Dermatitis:
- Results from excessive oil production on the skin.
- Commonly manifests as dandruff on the scalp, but can also affect the face, chest, and creases of arms, legs, or groin.
- Reaction to a normal yeast that grows on the skin.
- Athlete’s Foot:
- Fungal infection causes dry, flaky skin on the soles of the feet.
- Also known as “ringworm” when the fungus grows on the body.
- External Factors:
- Dry weather conditions, hot water, and certain chemicals can lead to skin dryness.
- Dermatitis Types:
- Contact Dermatitis: Develops when the skin reacts to substances, leading to localized inflammation.
- Irritant Contact Dermatitis: Caused by exposure to irritating chemicals like bleach.
- Allergic Contact Dermatitis: Results from exposure to allergens such as nickel.
- Seborrheic Dermatitis: Occurs due to excessive oil production, often causing a red and scaly rash on the scalp.
- Atopic Dermatitis (Eczema): Chronic skin condition causing dry, scaly patches, common among young children.
- Contact Dermatitis: Develops when the skin reacts to substances, leading to localized inflammation.
- Other Causes:
- Conditions like psoriasis and type 2 diabetes can contribute to skin dryness.
What are the symptoms of dry skin?
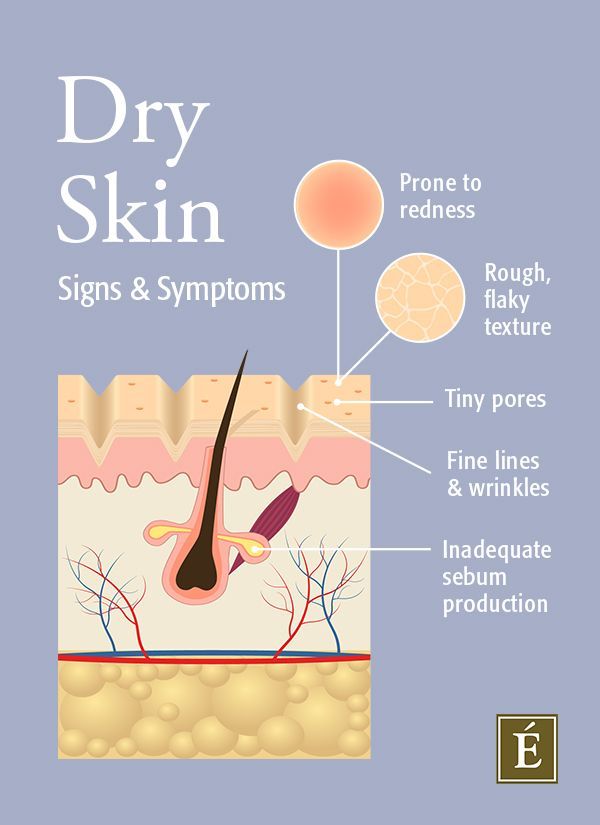
- Texture Changes:
- Cracked
- Rough
- Tight
- Flaking
- Scaling
- Color Changes:
- Lighter or darker than normal skin tone
- Red to purple
- Additional Symptoms for Severe Dry Skin:
- Rash development
- Small, pimple-like bumps
- Itchiness
- Swelling
- Altered color (usually red to purple)
- Dermatitis, indicating skin swelling and inflammation
- Markers for Treatment or Lifestyle Changes:
- Flaky or rough skin texture
- Excessive itchiness
- Susceptibility to infections
- Skin burns or stings
- Peeling skin
- Variability in Presentation:
- Rough, scaly, or flaky skin
- Mild to moderate itching
- Cracking skin with potential bleeding
- Chapped or cracked lips
- Common Areas Affected:
- The problem is often more pronounced on the arms and legs.
What are Causes and Factors Contributing to Dry Skin?

- Moisture Depletion in Skin Layers:
- Lack of moisture within skin layers results in dry skin.
- Age-Related Factors:
- Aging causes a reduction in oil gland activity, leading to decreased fat and collagen, resulting in thinner skin.
- Climate Influence:
- Environments with low humidity, such as desert-like or cold climates, contribute to dry skin.
- Winter conditions exacerbate dry skin, but it can occur year-round.
- Health Conditions and Genetics:
- Genetic predisposition or health conditions like allergies, eczema, diabetes, and kidney disease can increase the risk of dry skin.
- Occupational Factors:
- Certain professions, especially those involving outdoor work, chemical exposure, or frequent handwashing, can contribute to dry skin.
- Examples include healthcare providers, hairstylists, and farmers.
- Causes and Risk Factors for Severe or Chronic Dry Skin:
- Medications, older age, vitamin deficiency, diabetes, thyroid disease, kidney disease, chemotherapy, anorexia, and skin barrier dysfunction.
- Environmental Influences:
- Use of harsh cleaning products, deodorant soaps, long, hot showers, and living in cold, dry places can strip oils from the skin, leading to dryness.
- Treatment and Prevention:
- Moisturizing regularly is a key practice to heal and prevent dry skin.
- Identifying underlying causes, such as allergies, irritation, sun exposure, face washing habits, dehydration, perioral dermatitis, rosacea, eczema, or psoriasis, is crucial for effective treatment.
- When to Seek Medical Attention:
- Excessive dryness persisting despite lifestyle changes may require medical evaluation.
- Skin issues around the mouth can be attributed to various factors, including allergies, weather conditions, sun exposure, face washing, dehydration, perioral dermatitis, and underlying medical conditions like rosacea, eczema, or psoriasis. Medical consultation is recommended for accurate diagnosis and treatment.
How can we Prevent and Relieve Dry Skin?

Bathing Habits:
- Use comfortably warm (not hot) water.
- Choose unscented soap with high-fat content or glycerin, avoiding scrubbing.
- Quick showers after workouts with mild soap for athletes.
Moisturization:
- Pat dry after bath/shower and immediately apply unscented moisturizer.
- Apply sunscreen or petroleum jelly for outdoor activities/swimming.
- Use a humidifier during dry winter months.
Moisturizer Selection:
- Use moisturizers with glycerin, urea, pyroglutamic acid, sorbitol, lactic acid, lactate salts, or alpha hydroxy acids.
- Avoid overusing antiperspirants and perfumes.
Lifestyle Changes:
- Adjust bathing frequency (shower every other day), and duration (less than 10 minutes), and use moisturizing soap.
- Pat, don’t rub, wet skin dry with a soft towel.
- Avoid itching or scrubbing dry skin patches.
Overall Lifestyle Practices:
- Stay hydrated by drinking plenty of water.
- Manage stress to alleviate skin conditions.
- Minimize sun exposure to prevent oil and moisture evaporation.
- Quit smoking to prevent nicotine-induced skin dryness.
Additional Measures:
- Cleanse with mild, fragrance-free, moisturizing non-soap cleanser.
- Moisturize immediately after bathing while the skin is damp.
- Use a humidifier to add moisture to the home environment.
What is Diagnosis?
If you consult a doctor for dry skin, they will typically conduct a thorough examination and inquire about your medical history. During the assessment, they may discuss the onset of your dry skin, factors that exacerbate or alleviate the condition, details about your bathing routine, and your current skincare practices.
To determine if an underlying medical issue is contributing to your dry skin, your doctor might recommend tests. Conditions such as hypothyroidism, which is characterized by an underactive thyroid, could be assessed to identify any potential systemic causes for dry skin. Additionally, your doctor may explore the possibility of other skin conditions like psoriasis or dermatitis that could manifest as dry skin.
Ultimately, the goal of these evaluations is to pinpoint the root cause of your dry skin and tailor a treatment plan accordingly. Seeking professional medical advice is crucial for an accurate diagnosis and the development of an effective management strategy.
What are some Effective treatments for dry skin?
- There are Eight ways Effective treatments for dry skin:-
- Hydration
- Nutrition
- Moisturize Regularly
- Gentle Skin Care
- Humidify Your Environment
- Protect Your Skin
- Lifestyle Adjustments
- Over-the-Counter Treatments
- Professional Treatments
- Hydration
Hydration Good hydration is crucial for maintaining health and proper bodily functions, including muscle, brain, and heart health. It helps to reduce the risk of infections, particularly urinary tract infections (UTIs), which can be dangerous, especially for the elderly. Older individuals and those in care settings are at a higher risk of dehydration due to factors like decreased thirst awareness and communication barriers. Ensuring adequate fluid intake is essential for preventing dehydration and its associated risks, making it a critical aspect of care for vulnerable populations.
Water, constituting over half of the human body’s weight, is indispensable for sustaining life and ensuring optimal health. The human body demands regular fluid intake to compensate for water loss through various physiological processes. This necessity underscores the importance of hydration, particularly in care settings where the stakes of dehydration can be significantly higher.
- The Essence of Hydration
Hydration is fundamental to maintaining bodily functions. It facilitates crucial processes, including nutrient transportation, body temperature regulation, and waste elimination. Moreover, adequate fluid intake is instrumental in cognitive function, directly impacting concentration, alertness, and overall mental performance. The recommended daily fluid intake of 6-8 cups varies with physical activity levels and environmental conditions, highlighting the dynamic nature of our hydration needs.
- Hydration’s Impact on Health
The consequences of dehydration extend beyond mere thirst, leading to fatigue, headaches, and impaired cognitive functions. These symptoms can detrimentally affect the quality of life and health outcomes. In the realm of healthcare, particularly among vulnerable populations such as the elderly and those with chronic conditions, the implications are even more profound.
- The Link Between Hydration and Urinary Tract Infections (UTIs)
Good hydration is pivotal in preventing urinary tract infections (UTIs), a common yet potentially severe health issue in care settings. Adequate fluid intake ensures regular urination, flushing out pathogens from the urinary tract before they can establish an infection. This preventive measure is crucial for older adults, who are at increased risk for UTIs due to physiological changes and coexisting health conditions.
- The Challenge of Hydration in Care Settings
Maintaining hydration in care environments presents unique challenges. Older adults, for example, may not recognize or communicate their thirst adequately, increasing their risk of dehydration. This risk is compounded by factors such as diminished kidney function, which affects the body’s ability to conserve water, and the prevalence of comorbidities that can exacerbate vulnerability to dehydration.
To combat dehydration risks in care settings, proactive measures are essential. These include:
- Regular Monitoring: Implementing routine checks for signs of dehydration can ensure early detection and intervention.
- Encouraging Fluid Intake: Making fluids readily available and encouraging regular consumption throughout the day can help maintain hydration levels. This may involve personalized approaches to cater to individual preferences and needs.
- Education and Awareness: Educating caregivers and patients about the signs of dehydration and the importance of regular fluid intake can foster a proactive approach to hydration.
- Adapting to Individual Needs: Tailoring hydration strategies to accommodate the specific health conditions and limitations of individuals is crucial for effectiveness.
Conclusion
Hydration plays a critical role in maintaining health and preventing infections, particularly UTIs, in care settings. The challenges of ensuring adequate fluid intake among vulnerable populations necessitate targeted strategies and vigilant monitoring. By prioritizing hydration, caregivers can significantly impact the well-being and quality of life of those in their care, underscoring the vital role of water in health and healing.
2. Nutrition
Good nutrition is pivotal at any stage of life, but it becomes even more critical as we age. Older adults experience a myriad of physical and metabolic changes that necessitate a careful approach to their diet to maintain health, prevent chronic diseases, and ensure a high quality of life. The essence of good nutrition for older adults can be distilled into several key components, each playing a crucial role in supporting their overall well-being.
- Importance of a Well-Balanced Diet
- Prevention of Chronic Diseases: Proper nutrition is vital in preventing or managing chronic diseases prevalent in older age, such as heart disease, diabetes, and osteoporosis. A balanced diet rich in fruits, vegetables, lean proteins, and whole grains, and low in saturated fats and sodium can mitigate the risk factors associated with these conditions.
- Supporting Mental Health: Nutritional deficiencies can exacerbate cognitive decline and mood disorders. Ensuring an adequate intake of essential vitamins and minerals supports brain health, potentially reducing the risk of depression and cognitive decline.
- Bone Health: Aging is associated with a loss of bone density, increasing the risk of fractures. Calcium and vitamin D are crucial for maintaining bone health, necessitating their adequate consumption through diet or supplements.
- Muscle Mass Preservation: Sarcopenia, or the loss of muscle mass and strength, is a common issue in older adults, contributing to increased frailty and falls. A diet with sufficient protein intake, alongside physical activity, can help preserve muscle mass and function.
- Immune Function: Adequate nutrition supports the immune system, reducing the risk of infections, which older adults are more susceptible to due to a naturally declining immune system.
- Components of a Well-Balanced Diet
- Fruits and Vegetables: These are high in vitamins, minerals, fiber, and antioxidants but low in calories, making them ideal for managing weight and reducing disease risk.
- Proteins: Essential for repairing cells and making new ones. Older adults should focus on lean sources like poultry, fish, beans, and legumes.
- Whole Grains: Rich in fiber, vitamins, and minerals, whole grains help maintain digestive health and lower the risk of heart disease.
- Dairy: Sources of calcium and vitamin D are crucial for bone health. Low-fat or fat-free options can provide these benefits without excessive saturated fat.
- Healthy Fats: Fats are necessary for brain health and energy. Sources of healthy fats include avocados, nuts, seeds, and fish rich in omega-3 fatty acids.
- Challenges in Achieving Good Nutrition
For older adults, especially those in care settings, achieving these dietary goals can be challenging due to various factors such as:
- Decreased mobility or physical issues that make cooking and eating difficult.
- Cognitive impairments lead to forgotten meals or poor dietary choices.
- Financial constraints limit access to a variety of healthy foods.
- Medications that affect appetite or nutrient absorption.
- Strategies for Improving Nutrition in Care
- Personalized Meal Plans: Tailoring nutrition plans to the individual’s health status, preferences, and dietary needs can improve intake and satisfaction.
- Education and Support: Educating caregivers and family members on the importance of nutrition and how to prepare balanced meals can enhance the dietary quality of older adults.
- Monitoring and Intervention: Regular screening for malnutrition and timely interventions can prevent or address nutritional deficiencies effectively.
- Accessibility to Healthy Options: Ensuring that healthy, appealing food choices are readily available and easy to consume can significantly improve nutritional intake.
Conclusion
In conclusion, nutrition is a cornerstone of health and well-being in elderly care, playing a vital role in maintaining physical health, cognitive function, and quality of life. Overcoming the challenges to good nutrition requires a concerted effort from individuals, caregivers, and healthcare providers to ensure that dietary needs are met with thoughtful, personalized approaches. As the population ages, prioritizing nutrition in care settings becomes increasingly critical in promoting longevity and reducing the burden of age-related diseases. By embracing the principles of good nutrition, we can help ensure that our elderly loved ones lead fulfilling, healthy lives.
3. Moisturize Regularly
The provides a comprehensive overview of the importance of moisturizers in daily skincare, especially in the context of skin barrier alteration and dryness-related dermatoses.
It discusses the various types of moisturizers, including emollients, occlusives, and humectants, along with their mechanisms of action and benefits. Additionally, it emphasizes the significance of proper moisturizer selection and application techniques, tailored to individual skin types and conditions.
The essay underscores the multifaceted roles of moisturizers, not only in hydrating the skin but also in improving its texture, reducing fine lines and wrinkles, soothing irritations, and creating a protective barrier against environmental stressors. Furthermore, it highlights the importance of using moisturizers as both cosmetics and therapeutic products, especially in managing dermatological conditions associated with dryness.
conclusion
In conclusion, the emphasizes the essential role of moisturizers in maintaining skin health and improving overall quality of life. It stresses the importance of regular moisturizer use, along with adopting good skin care habits, to address dry skin concerns effectively. Additionally, it encourages seeking medical advice if persistent dryness persists, underscoring the importance of dermatological guidance in skincare routines.
4. Gentle Skin Care
Maintaining a skincare routine tailored to dry skin is essential for keeping it hydrated and protected from the elements. The routine typically involves steps such as cleansing, toning, using serums, applying eye cream, moisturizing, and using sunscreen during the day. At night, the focus shifts to removing impurities, adding hydration, and repairing the skin while you sleep.
Key Components
- Cleansing: Use gentle cleansers, oil-based cleansers, or moisturizing cleansers to remove dirt without stripping away essential oils.
- Toning: Opt for alcohol-free toners with hydrating ingredients like hyaluronic acid and vitamin E to refresh and cleanse without over-drying.
- Serums: Look for serums with hydrating ingredients such as hyaluronic acid, niacinamide, and ceramides to replenish moisture and enhance the skin barrier.
- Eye Cream: Use hydrating eye creams with peptides and antioxidants like Vitamin C to moisturize and protect the delicate under-eye area.
- Moisturizer: Apply rich moisturizers with ingredients like ceramides, niacinamide, and hyaluronic acid to repair the skin barrier and lock in moisture.
- Sunscreen: End your morning routine with sunscreen to protect dry skin from UV rays.
Conclusion
Having a consistent skincare routine for dry skin can significantly improve its texture and overall health. By incorporating hydrating products and protective measures, you can effectively combat dryness, flakiness, and sensitivity. Additionally, experimenting with different products and finding what works best for your skin type is crucial for achieving optimal results.
5. Humidify Your Environment
The benefits of using a humidifier for skin health, particularly in terms of hydrating the skin, reducing flare-ups of conditions like eczema, and potentially reducing breakouts. It also explains how humidifiers work, and who could benefit from using one and offers tips for proper usage and maintenance.
The effects of both high and low humidity levels on the skin, highlight how high humidity can help maintain hydration, promote skin cell turnover, and potentially have anti-aging effects, while low humidity can lead to dryness, dead skin cell buildup, and exacerbation of skin conditions like eczema.
- Humidifiers can help maintain skin hydration, especially in dry climates or during winter months.
- They may reduce flare-ups of conditions like eczema and improve overall skin quality.
- Proper maintenance and cleaning of humidifiers are crucial to prevent the growth of harmful microorganisms.
- While humidifiers can be beneficial, they should not replace a consistent skincare routine.
- High humidity levels can benefit dry or normal skin but may exacerbate issues for oily skin, leading to increased sebum production and potentially acne.
- Low humidity levels can cause dryness, dead skin cell buildup, and worsen skin conditions like eczema.
- Tips for skincare in high humidity include regular exfoliation and using lightweight moisturizers, while in low humidity, thicker moisturizers and humidifiers can help maintain skin hydration.
Conclusion
In conclusion, humidifiers can play a significant role in maintaining skin health, especially in environments with low humidity. However, they should be used in conjunction with a consistent skincare routine, as they cannot treat underlying skin conditions on their own. Proper maintenance and cleanliness of the humidifier are crucial to prevent the growth of harmful microorganisms. Additionally, individuals should be mindful of their skin type and environmental factors to determine the most suitable skincare routine. Overall, using a humidifier appropriately can contribute to healthier, more hydrated skin.
6. Protect Your Skin
Protecting your skin from indoor heating and the harsh winter weather is essential to maintain its health and appearance. Here are some key tips to consider:
- Moisturize often with products suitable for cold and dry weather to keep your skin hydrated and nourished.
- Invest in a humidifier to add moisture to the air and prevent your skin from drying out due to indoor heating.
- Use nourishing face masks, such as those containing honey, to replenish your skin’s moisture and restore its radiance.
- Maintain a consistent skincare routine tailored to your skin type to protect it from environmental stressors and slow down aging.
- Avoid long hot showers, as they can strip away moisture from your skin, and opt for lukewarm water instead.
- Switch to fragrance-free skincare and laundry products to avoid irritating your skin further.
- Incorporate home remedies like coconut oil, yogurt, and honey to soothe and hydrate dry and flaky skin.
Conclusion
Protecting your skin from the harsh effects of indoor heating and winter weather requires a proactive approach. By following these tips and incorporating them into your skincare routine, you can keep your skin healthy, hydrated, and radiant throughout the colder months. Remember to choose products and practices that suit your skin type and address your specific concerns to achieve the best results. With consistency and care, you can effectively manage dry and flaky skin and enjoy a comfortable and glowing complexion all year round.
7. Lifestyle Adjustments
Achieving healthy, vibrant skin doesn’t have to involve complicated skincare routines or expensive products. By making simple lifestyle changes, you can significantly improve the health and appearance of your skin. Some key changes include maintaining a balanced diet rich in fruits, vegetables, lean proteins, and healthy fats while avoiding simple carbohydrates and staying hydrated. Prioritize hydration, protect your skin from UV damage, and be mindful of water temperature during showers. Incorporate green tea, coconut oil, and regular exercise into your routine, and make sleep a priority for skin cell regeneration. Consider LED skin treatments and consult a dermatologist for persistent issues. Additionally, managing stress, improving air quality, and reducing dairy intake can contribute to healthier skin. Develop a personalized skincare routine tailored to your skin type to ensure optimal results.
Conclusion
Healthy, vibrant skin is achievable through simple lifestyle modifications that prioritize hydration, nutrition, protection from environmental factors, and stress management. By incorporating these changes into your daily routine and adopting a personalized skincare regimen, you can enhance the health and appearance of your skin, promoting a radiant complexion and overall well-being. Remember, consistency is key, and with dedication to these practices, you can enjoy the benefits of beautiful skin for years to come.
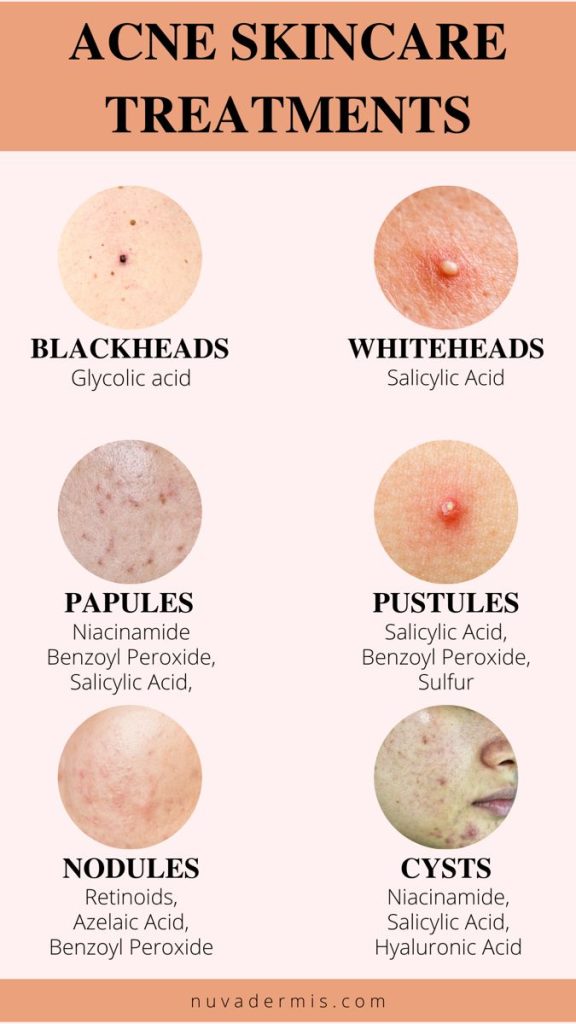
8. Over-the-counter treatments
The over-the-counter (OTC) treatments for eczema, focus on four main categories: lotions and moisturizers, oral antihistamines and pain relievers, topical hydrocortisone, and shampoos. Lotions and moisturizers are recommended to prevent dry skin and reduce eczema symptoms. Oral antihistamines and pain relievers can provide relief from itching and inflammation, particularly for those with allergies or sensitive skin. Topical hydrocortisone creams help reduce irritation and inflammation but may cause side effects if not used properly. Medicated shampoos can address symptoms of seborrheic dermatitis on the scalp. Additionally, the article briefly mentions home remedies for dry skin.
Conclusion
Conclusion: Eczema treatment often involves a combination of prescribed medication and over-the-counter products. OTC treatments like lotions, antihistamines, hydrocortisone creams, and shampoos can provide relief from eczema symptoms and help manage flare-ups. However, it’s important to use these products as directed and consult a healthcare provider if symptoms persist or worsen. Additionally, incorporating home remedies and proper skincare practices can further support overall skin health and comfort, especially in managing dryness associated with eczema.
9. Professional Treatments
It seems like you’ve provided additional information about professional skincare treatments for dry skin, including SkinCeuticals Micropeel Sensitive. Here’s a summary of the treatments mentioned:
- Laser Genesis: This treatment uses microsecond pulses to heat the skin, stimulating collagen and elastin production. It can improve wrinkles, scarring, and redness with minimal downtime.
- Skin Needling (Microneedling): Involves puncturing the skin with micro-needles to stimulate collagen and elastin production, reducing wrinkles, fine lines, and improving skin texture and tone.
- HydraFacial MD: A non-invasive facial treatment that deeply hydrates the skin, cleanses pores, and infuses antioxidants, peptides, and hyaluronic acid into the skin for a smoother, plumper, and brighter complexion.
- Dermaplaning: This treatment involves using a scalpel to remove vellus hair and the outer layer of dead skin cells, improving product penetration and skin texture while softening fine lines and wrinkles.
- SkinCeuticals Micropeel Sensitive: A superficial peel utilizing lactic acid and niacin to exfoliate and polish the skin, reducing sun damage and congestion. It can be paired for enhanced results and can be performed every 4 to 6 weeks.
Conclusion
To complement professional treatments, it’s recommended to use high-quality skincare products containing ingredients like vitamin B3, vitamin C, vitamin A, and hyaluronic acid to maintain skin hydration and health. Additionally, avoid drying products and always use sunscreen to protect the skin from sun damage. Consistent skincare routines at home are also crucial for maintaining the results of professional treatments.