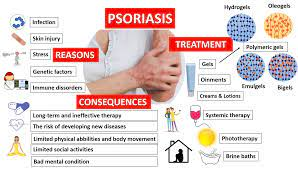
Psoriasis is a chronic autoimmune condition characterized by the rapid buildup of skin cells, leading to the development of thick, red, and scaly patches on the skin. Treatment for psoriasis aims to reduce inflammation, control symptoms, and improve the quality of life for individuals affected by the condition. It’s important to note that the effectiveness of treatments can vary from person to person, and what works for one individual may not work as well for another.
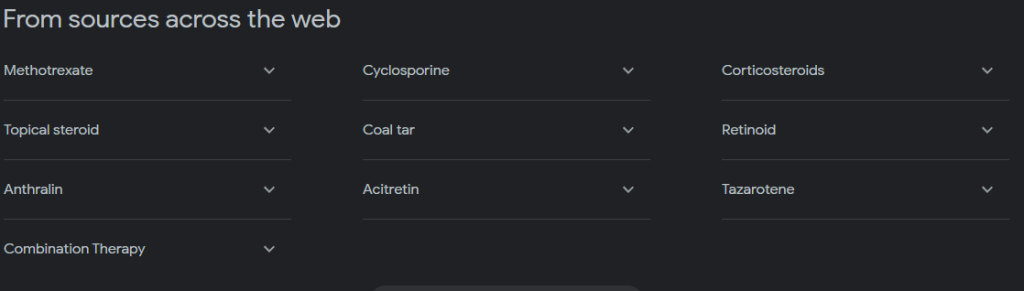
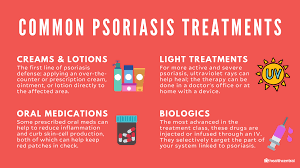
1.Topical Treatments:-
1.Corticosteroids: Corticosteroids, also known simply as steroids, are a class of medications that mimic the effects of hormones produced by the adrenal glands, particularly cortisol. These medications have potent anti-inflammatory properties and are used to treat a variety of inflammatory conditions, including psoriasis. Corticosteroids can be classified into two main types based on their potency: topical (applied to the skin) and systemic (taken internally).
Your health care provider may prescribe a stronger corticosteroid cream or ointment — triamcinolone (Trianex) or clobetasol (Cormax, Temovate, others) — for smaller, less-sensitive or tougher-to-treat areas.
Long-term use or overuse of strong corticosteroids can thin the skin. Over time, topical corticosteroids may stop working.
- How they work: These are creams, ointments, gels, or lotions that are applied directly to the skin. They work by reducing inflammation, suppressing the immune response, and slowing down the rapid growth of skin cells.
- Effectiveness: Topical corticosteroids are often effective in managing mild to moderate psoriasis symptoms, such as redness, itching, and scaling.
2.Topical retinoids: Topical retinoids are not typically considered a first-line treatment for psoriasis, as they are more commonly used for conditions like acne. Psoriasis is an autoimmune skin condition characterized by the rapid production of skin cells, leading to the development of red, scaly patches. Topical corticosteroids, vitamin D analogs, and other medications are often preferred for managing psoriasis.
- Tazarotene isn’t recommended when you’re pregnant or breastfeeding or if you intend to become pregnant.
- Cellular Differentiation: Retinoids influence the differentiation of skin cells, encouraging normal maturation. In psoriasis, skin cells (keratinocytes) tend to mature and proliferate more rapidly than normal, leading to the characteristic plaques and scales. By promoting more regular differentiation, retinoids may help normalize this process.
- Anti-inflammatory Effects: Tazarotene has been shown to have anti-inflammatory properties. Psoriasis is an inflammatory skin condition, and by reducing inflammation, retinoids may help alleviate symptoms.
- Inhibition of Hyperproliferation: Psoriasis is characterized by an abnormal increase in the production of skin cells. Retinoids may help regulate this hyperproliferation, leading to a reduction in the thickening and scaling of the skin seen in psoriasis plaques.
3.Calcineurin inhibitors: Calcineurin inhibitors, specifically tacrolimus and pimecrolimus, are a class of medications that have been used to treat inflammatory skin conditions, including psoriasis. These medications are typically applied topically and are considered for use in areas where other treatments may be less suitable, such as on the face and intertriginous areas (areas where skin rubs against skin, such as the armpits or groin).
Mechanism of Action:
- Inhibition of Calcineurin: Tacrolimus and pimecrolimus work by inhibiting calcineurin, a cellular enzyme involved in the activation of T-lymphocytes (immune cells). By inhibiting calcineurin, these medications interfere with the inflammatory cascade that contributes to the development of psoriasis plaques.
- Modulation of Immune Response: Psoriasis is an autoimmune condition where the immune system mistakenly attacks healthy skin cells. Calcineurin inhibitors help modulate the immune response, reducing the excessive activation of immune cells and the subsequent inflammation in the skin.
Effectiveness:
The effectiveness of calcineurin inhibitors for psoriasis can vary from person to person. These medications are generally considered when other topical treatments, such as corticosteroids, may not be suitable for certain areas of the body. Some key points regarding the use of calcineurin inhibitors for psoriasis include:
- Facial and Intertriginous Areas: Calcineurin inhibitors are often preferred for treating psoriasis on the face, neck, and in skin folds where the skin is more sensitive.
- Maintenance Therapy: They may be used as maintenance therapy to manage psoriasis in areas where long-term use of other medications, like topical steroids, might lead to side effects.
- Avoiding Steroid-related Side Effects: Since calcineurin inhibitors work through a different mechanism than corticosteroids, they can be an option for individuals who need to avoid the potential side effects associated with prolonged use of steroids, such as skin thinning.
4.Vitamin D analogues: Vitamin D analogues are a class of medications commonly used in the treatment of psoriasis. These synthetic forms of vitamin D help regulate the growth and development of skin cells, which is particularly relevant in the context of psoriasis where there is an abnormal acceleration of skin cell turnover. Two commonly used vitamin D analogues for psoriasis are calcipotriene and calcitriol.
Mechanism of Action:
- Regulation of Cell Growth: Vitamin D analogues work by binding to vitamin D receptors on skin cells. This binding helps regulate the growth and maturation of these cells, preventing the excessive proliferation seen in psoriasis.
- Anti-inflammatory Effects: Vitamin D analogues also have anti-inflammatory properties. Psoriasis is characterized by inflammation, and these medications can help reduce the inflammatory response in the skin.
Effectiveness:
- Mild to Moderate Psoriasis: Vitamin D analogues are often used in the treatment of mild to moderate psoriasis, either alone or in combination with other topical treatments.
- Scalp Psoriasis: Calcipotriene, in particular, is commonly used for treating scalp psoriasis. It is available in both solution and foam formulations for easier application to the scalp.
- Combination Therapy: Vitamin D analogues are sometimes used in combination with topical corticosteroids for enhanced effectiveness. Combining these medications can provide the benefits of both anti-inflammatory effects and regulation of cell growth.
- Long-Term Maintenance: Vitamin D analogues can be used for long-term maintenance therapy to help control psoriasis and prevent flare-ups.
5. Salicylic acid: Salicylic acid is a common topical treatment for psoriasis and other skin conditions. It is often used in conjunction with other therapies, and its main function is to help remove scales and promote the penetration of other medications.
Mechanism of Action:
- Scale Removal: Salicylic acid is a keratolytic agent, meaning it helps to soften and remove scales (dead skin cells) that are common in psoriasis plaques. This can help reduce the thickness of the plaques and improve the appearance of the skin.
- Enhanced Penetration: By breaking down the outer layer of skin, salicylic acid can enhance the penetration of other topical medications, allowing them to be more effective.
Effectiveness:
- Scale Reduction: Salicylic acid is particularly useful in addressing the scaling associated with psoriasis. It helps to exfoliate the skin and reduce the buildup of dead cells.
- Combination Therapy: It is often used in combination with other topical treatments, such as corticosteroids or vitamin D analogues. Combining salicylic acid with these medications can improve their efficacy.
- Scalp Psoriasis: Salicylic acid is commonly found in shampoos formulated for scalp psoriasis. These shampoos can help lift and remove scales from the scalp.
6. Coal tar: Coal tar has been used for many years in the treatment of psoriasis due to its anti-inflammatory, antipruritic (anti-itch), and keratolytic (scale-softening) properties. It is available in various formulations, including shampoos, creams, ointments, and solutions.
Mechanism of Action:
- Anti-Inflammatory: Coal tar has mild anti-inflammatory effects, helping to reduce the redness and swelling associated with psoriasis.
- Antipruritic: It helps relieve itching, which is a common symptom of psoriasis.
- Keratolytic: Coal tar helps to slow down the rapid growth of skin cells, promoting a more normal skin cell turnover. This can help reduce the thickness of psoriasis plaques and scales.
Effectiveness:
- Scaling and Itching: Coal tar is particularly effective in reducing scaling and itching associated with psoriasis.
- Plaque Thickness: It can help decrease the thickness of psoriasis plaques, making them less prominent.
- Chronic Maintenance: Coal tar is often used for long-term maintenance therapy to manage psoriasis and prevent flare-ups.
Anthralin: Anthralin is another topical treatment option for psoriasis, particularly for plaque psoriasis. It has been used for many years and is effective in slowing down the growth of skin cells and reducing inflammation.
Mechanism of Action:
- Anti-Proliferative: Anthralin slows down the excessive growth of skin cells (keratinocytes) that occurs in psoriasis. This helps to normalize the rate of cell turnover.
- Anti-Inflammatory: Anthralin has anti-inflammatory properties, which can help reduce redness and swelling associated with psoriasis.
Effectiveness:
- Scaling and Plaque Thickness: Anthralin is effective in reducing scaling and the thickness of psoriasis plaques.
- Chronic Maintenance: It is often used for long-term maintenance therapy to manage psoriasis and prevent flare-ups.
2. Phototherapy(Light therapy)

Phototherapy, or light therapy, is a treatment for psoriasis that involves exposing the skin to ultraviolet (UV) light. This form of therapy is often considered when topical treatments alone are not sufficient and before systemic medications are prescribed. Phototherapy can be conducted in various settings, including medical facilities or under the guidance of healthcare professionals, and it can also be administered at home using special devices.
1.UVB broadband: UVB (ultraviolet B) broadband phototherapy is a commonly used treatment for psoriasis, a chronic skin condition characterized by red, itchy, and scaly patches. UVB therapy involves exposing the skin to artificial UVB light to slow down the growth of affected skin cells. UVB light is part of the ultraviolet spectrum and is found in natural sunlight.
UVB (ultraviolet B) broadband phototherapy is a commonly used treatment for psoriasis, a chronic skin condition characterized by red, itchy, and scaly patches. UVB therapy involves exposing the skin to artificial UVB light to slow down the growth of affected skin cells. UVB light is part of the ultraviolet spectrum and is found in natural sunlight.
Broadband UVB therapy uses a broader spectrum of UVB light, including both shorter and longer wavelengths. This is in contrast to narrowband UVB therapy, which uses a more specific range of UVB light. Both types of UVB therapy have been shown to be effective in treating psoriasis.
UVB therapy works by penetrating the skin and slowing down the rapid growth of skin cells associated with psoriasis. It also has anti-inflammatory effects. UVB treatment can be administered in various ways:
- UVB Phototherapy Units: These units emit UVB light and can be used in a clinic or at home. The exposure time and intensity are carefully controlled to avoid overexposure and minimize side effects.
- UVB Booths: Larger units that allow for exposure of the entire body. These are often used in clinical settings.
- Handheld UVB Devices: These smaller devices are suitable for treating specific areas of the body.
2.UVB narrowband: UVB narrowband phototherapy is a well-established and effective treatment for psoriasis.In many places it has replaced broadband therapy. It’s usually administered two or three times a week until the skin improves and then less frequently for maintenance therapy. But narrowband UVB phototherapy may cause more-severe side effects than UVB broadband.
Effectiveness: Narrowband UVB therapy has been found to be highly effective in treating psoriasis, often producing significant improvement in symptoms. It is considered a first-line treatment for moderate to severe psoriasis, especially when other topical treatments have not provided sufficient relief.
Side Effects: While UVB narrowband therapy is generally well-tolerated, potential side effects may include redness, itching, and dryness. These side effects are usually mild and temporary.
3. Goeckerman therapy: Goeckerman therapy is a combination treatment for psoriasis that involves the use of coal tar and ultraviolet B (UVB) phototherapy. This therapy is named after Dr. William H. Goeckerman, who developed it in the early 20th century. Goeckerman therapy has been found to be effective, especially for individuals with moderate to severe psoriasis.
Treatment Schedule: Goeckerman therapy is typically administered in a medical setting, such as a dermatologist’s office or a specialized clinic. Treatment sessions are usually given three to five times per week. The duration of each session and the overall length of the treatment course can vary based on the severity of the psoriasis and the individual’s response to therapy.
Monitoring: Throughout the course of Goeckerman therapy, patients are closely monitored by healthcare professionals to assess progress and manage any potential side effects. Adjustments to the treatment plan may be made as needed.
4.Psoralen plus ultraviolet A (PUVA): Psoralen plus ultraviolet A (PUVA) therapy is another treatment option for psoriasis, particularly for individuals with moderate to severe cases that haven’t responded well to other treatments. PUVA involves the use of a photosensitizing medication called psoralen in combination with ultraviolet A (UVA) light exposure. Psoralen makes the skin more sensitive to UVA, enhancing the therapeutic effects of the ultraviolet light.
Psoralen Medication: Psoralen is typically administered either orally (as a pill) or topically (as a bath or lotion) before UVA exposure. The medication makes the skin more responsive to UVA light.
Treatment Schedule: PUVA therapy is usually administered two to three times per week. The frequency and duration of treatment sessions depend on factors such as the severity of the psoriasis and individual response to therapy. Over time, the frequency of treatments may be reduced as the condition improves.
Effectiveness: PUVA therapy has been shown to be effective in treating psoriasis, particularly for individuals with extensive or stubborn plaques. It can be used for various forms of psoriasis, including plaque psoriasis, guttate psoriasis, and palmoplantar psoriasis.
5.Excimer laser: Excimer laser therapy is a targeted and effective treatment for psoriasis, particularly for localized psoriatic plaques. This type of laser therapy uses a 308-nanometer wavelength of ultraviolet B (UVB) light, which is the same wavelength that is effective in traditional UVB phototherapy. The excimer laser delivers a highly focused beam of UVB light directly to the affected skin, avoiding exposure to surrounding healthy skin.
Targeted Treatment: The excimer laser allows for precise targeting of psoriatic lesions without affecting healthy skin. This targeted approach can be especially beneficial for individuals with localized plaques, such as those on the elbows, knees, or scalp.
Treatment Sessions: Excimer laser therapy typically involves a series of short treatment sessions, with the number of sessions and the duration of each session depending on factors such as the severity of the psoriasis and the individual’s response to treatment. Sessions are usually performed two to three times per week.
Quick Treatment: Each treatment session is relatively short, typically lasting only a few minutes. This makes excimer laser therapy a convenient option for individuals with busy schedules.
Effectiveness: Excimer laser therapy has been shown to be effective in improving psoriasis symptoms, including reducing redness, scaling, and thickness of plaques. Many individuals experience significant improvement after a few sessions.
Oral or injected medications:Oral and injected medications are often prescribed for individuals with moderate to severe psoriasis or when other treatments have not provided sufficient relief. These medications work systemically, targeting the underlying causes of psoriasis and modulating the immune system to reduce inflammation and slow down the abnormal growth of skin cells.
Methotrexate (Oral/Injected):
- Administration: Methotrexate can be taken orally in pill form or administered as an injection.
- Mechanism of Action: It suppresses the immune system and reduces the overgrowth of skin cells.
- Monitoring: Regular blood tests are necessary to monitor liver function and other potential side effects.
Cyclosporine (Oral):
- Administration: Cyclosporine is taken orally in pill form.
- Mechanism of Action: It suppresses the immune system to reduce inflammation.
- Monitoring: Regular monitoring of blood pressure and kidney function is essential due to potential side effects.
Acitretin (Oral):
- Administration: Acitretin is taken orally in pill form.
- Mechanism of Action: It is a retinoid that helps control the growth of skin cells.
- Monitoring: Regular monitoring of lipid levels and liver function is necessary.
Biologics (Injected):
- Administration: Biologics are administered through injections, either subcutaneous or intravenous.
- Types: Biologics include TNF-alpha inhibitors (e.g., adalimumab, etanercept), IL-17 inhibitors (e.g., secukinumab, ixekizumab), IL-12/IL-23 inhibitors (e.g., ustekinumab), and others.
- Mechanism of Action: They target specific immune system components involved in the inflammatory process.
- Monitoring: Regular monitoring for potential side effects, including infections, is important.
IL-23 Inhibitors (Injected):
- Administration: These medications are injected subcutaneously.
- Types: Medications like guselkumab and risankizumab target IL-23, a protein involved in the inflammatory response.
- Mechanism of Action: They specifically target the IL-23 pathway to reduce inflammation.
- Monitoring: Regular monitoring for potential side effects is necessary.
Apremilast (Oral):
- Administration: Apremilast is taken orally in pill form.
- Mechanism of Action: It inhibits an enzyme involved in the inflammatory process.
- Monitoring: Regular monitoring for potential side effects, including gastrointestinal symptoms, is important.
3. Alternative medicine

While conventional medical treatments are often recommended for managing psoriasis, some individuals explore alternative or complementary approaches to supplement their care. It’s important to note that the effectiveness of alternative treatments can vary, and not all of them have strong scientific evidence supporting their efficacy. Here are some alternative approaches that individuals with psoriasis may consider, but it’s crucial to consult with a healthcare professional before trying any new treatment.
1.Dietary Changes:
- Anti-Inflammatory Diet: Some people with psoriasis find relief by following an anti-inflammatory diet, which typically includes fruits, vegetables, whole grains, and omega-3 fatty acids while limiting processed foods, red meat, and dairy.
- Gluten-Free Diet: Some individuals with psoriasis and gluten sensitivity or celiac disease may benefit from a gluten-free diet.
2.Supplements:
- Fish Oil: Omega-3 fatty acids found in fish oil may have anti-inflammatory effects and could potentially benefit individuals with psoriasis.
- Vitamin D: Adequate vitamin D levels may be important for skin health, and some people with psoriasis may consider vitamin D supplements.
3.Herbal Remedies:
- Aloe Vera: Aloe vera gel, applied topically, may provide soothing relief for some individuals with psoriasis.
- Turmeric: Curcumin, the active component in turmeric, has anti-inflammatory properties and may be beneficial for some people. It can be taken as a supplement or included in the diet.
4. Topical Applications:
- Oats: Oatmeal baths or oat-based creams may help soothe irritated skin.
- Apple Cider Vinegar: Some people use diluted apple cider vinegar as a topical treatment, but caution is needed as it may cause skin irritation in some individuals.
5. Mind-Body Therapies:
- Stress Management: Techniques such as meditation, yoga, or deep breathing exercises may help manage stress, which can be a trigger for psoriasis flares in some individuals.
6. Acupuncture:
- Some individuals find acupuncture, an ancient Chinese practice involving the insertion of thin needles into specific points on the body, to be a complementary approach for managing psoriasis symptoms.