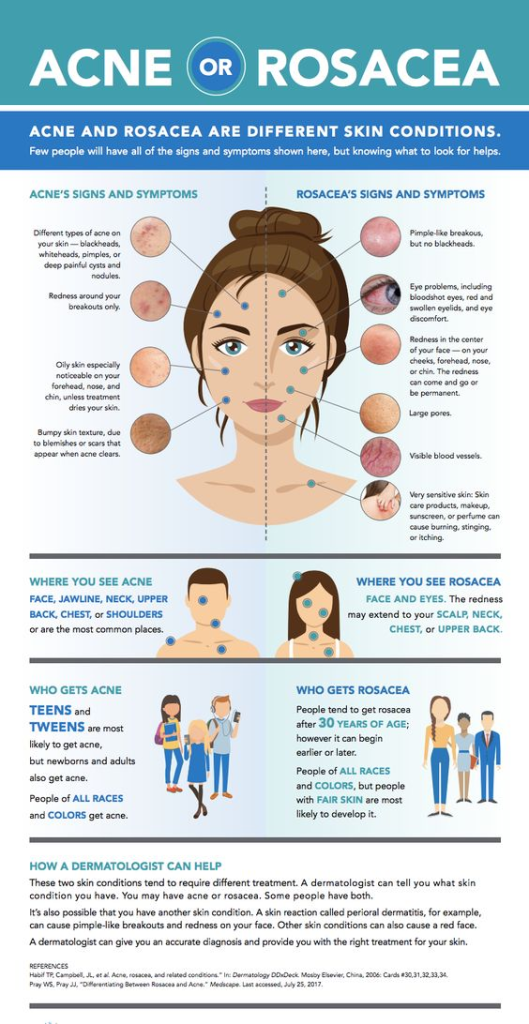
Rosacea is a skin condition characterized by flushed or red skin, often accompanied by small pus-filled bumps, resembling acne. Symptoms can vary based on skin color, with flushing being more noticeable on lighter skin. However, it may be harder to diagnose in individuals with brown or Black skin. Even without obvious redness, signs of rosacea include small red bumps, pus-filled bumps, and sensations like stinging, burning, and sensitivity. Seeking medical advice is essential for an accurate diagnosis. Treatment options, including medication and home care measures, can help manage symptoms and improve the condition.
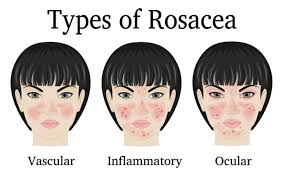
Rosacea Types
Erythematotelangiectatic Rosacea (ETR):
- Erythematotelangiectatic rosacea is characterized by persistent redness on the face. Small blood vessels beneath the skin surface may become enlarged and visible; these symptoms often flare up and then disappear. Persistent redness (erythema) on the central part of the face, including the cheeks, nose, forehead, and chin. Visible blood vessels (telangiectasias) may also be present. Without treatment, the redness can get more persistent, cover more skin, and even become permanent. Flushing and a tendency to blush easily. The skin may be sensitive and stinging.
- Symptoms:(i)Redness: Individuals with PPR experience persistent redness on the central part of the face, including the cheeks, nose, forehead, and chin.(ii)Papules and Pustules: PPR is distinguished by the presence of inflammatory papules and pustules, which can be mistaken for acne. These bumps may come and go, and they may be accompanied by a burning or stinging sensation.
- Flushing and Blushing: People with PPR often have a tendency to flush or blush easily. Flushing episodes can be triggered by various factors such as spicy foods, alcohol, temperature changes, or emotional stress.
- Sensitivity and Stinging: The skin in individuals with PPR is often sensitive and may experience a stinging sensation. Harsh skincare products and environmental factors can contribute to skin irritation.
- Triggers: Common triggers for PPR include exposure to sunlight, hot drinks, spicy foods, alcohol, stress, and certain medications.
- Differential Diagnosis: PPR is sometimes referred to as “acne rosacea” due to its appearance, but it is distinct from acne. While both conditions involve facial bumps, they have different underlying causes and require different treatments.
- Treatment: Treatment for PPR aims to reduce inflammation, control papules, and pustules, and alleviate associated symptoms. Dermatologists may prescribe topical medications, oral antibiotics, or a combination of both, depending on the severity of symptoms.
- Skincare and Lifestyle Management: Avoiding triggers, using gentle skincare products, and protecting the skin from sun exposure are important aspects of managing PPR. Individuals with rosacea, including PPR, should be cautious about skincare routines and choose products that are suitable for sensitive skin.
Papulopustular Rosacea (PPR):
- Papulopustular Rosacea (PPR): Papulopustular Rosacea (PPR) is one of the subtypes of rosacea, a chronic skin condition that primarily affects the face. PPR is characterized by a combination of persistent redness, visible blood vessels (telangiectasias), and the presence of papules (small red bumps) and pustules (pus-filled bumps) on the skin.
- Symptoms:Redness:(i) Individuals with PPR experience persistent redness on the central part of the face, including the cheeks, nose, forehead, and chin.(ii)Papules and Pustules: PPR is distinguished by the presence of inflammatory papules and pustules, which can be mistaken for acne. These bumps may come and go, and they may be accompanied by a burning or stinging sensation.
- Flushing and Blushing: People with PPR often have a tendency to flush or blush easily. Flushing episodes can be triggered by various factors such as spicy foods, alcohol, temperature changes, or emotional stress.
- Sensitivity and Stinging: The skin in individuals with PPR is often sensitive and may experience a stinging sensation. Harsh skincare products and environmental factors can contribute to skin irritation.
- Triggers: Common triggers for PPR include exposure to sunlight, hot drinks, spicy foods, alcohol, stress, and certain medications.
- Differential Diagnosis: PPR is sometimes referred to as “acne rosacea” due to its appearance, but it is distinct from acne. While both conditions involve facial bumps, they have different underlying causes and require different treatments.
- Treatment: Treatment for PPR aims to reduce inflammation, control papules and pustules, and alleviate associated symptoms. Dermatologists may prescribe topical medications, oral antibiotics, or a combination of both, depending on the severity of symptoms.
- Skincare and Lifestyle Management: Avoiding triggers, using gentle skincare products, and protecting the skin from sun exposure are important aspects of managing PPR. Individuals with rosacea, including PPR, should be cautious about skincare routines and choose products that are suitable for sensitive skin.
Phymatous Rosacea:
Phymatous rosacea is a subtype of rosacea, a chronic skin condition that primarily affects the face. This particular subtype is characterized by the thickening of the skin and the development of irregular surface nodularities. Phymatous rosacea often affects the nose (rhinophyma), but it can also occur on the chin, forehead, cheeks, or ears.
- Thickening of the Skin: The hallmark feature of phymatous rosacea is the thickening of the skin. This thickening can lead to a bulbous and swollen appearance in the affected areas.
- Rhinophyma: Rhinophyma is the most common manifestation of phymatous rosacea and involves the thickening of the skin on the nose. This can result in a bulbous and enlarged appearance of the nose.
- Irregular Surface Nodularities: The skin affected by phymatous rosacea may develop irregular surface nodularities, creating an uneven texture.
- Enlargement of Sebaceous Glands: Phymatous rosacea is associated with the enlargement of sebaceous (oil) glands in the affected areas. This contributes to the thickening and swelling of the skin.
- Progression Over Time: Phymatous rosacea tends to develop gradually over time, and the severity can vary from person to person. It is more commonly seen in men than in women.
- Other Subtypes: Phymatous rosacea can occur in conjunction with other subtypes of rosacea, such as Erythematotelangiectatic Rosacea (ETR) or Papulopustular Rosacea (PPR). In some cases, individuals may experience a combination of symptoms from different subtypes.
- Treatment: Treatment for phymatous rosacea often involves a combination of medical and surgical approaches. Surgical interventions may be considered to address the thickened skin and nodularities. Dermatologists may also recommend oral antibiotics or isotretinoin to manage inflammation.
- Monitoring and Care: Regular monitoring by a dermatologist is important to assess the progression of phymatous rosacea and to adjust the treatment plan as needed. Sun protection and gentle skincare are also crucial components of care.
Ocular Rosacea:
Ocular Rosacea is a subtype of rosacea that affects the eyes. It involves inflammation of the eyes and the eyelids and can lead to a range of ocular symptoms. Ocular rosacea often occurs in conjunction with other subtypes of rosacea, such as Erythematotelangiectatic Rosacea (ETR) or Papulopustular Rosacea (PPR).
- Ocular Symptoms: Ocular rosacea primarily affects the eyes and can cause a variety of symptoms, including redness, dryness, burning, itching, and the sensation of a foreign body in the eyes.
- Blepharitis: Inflammation of the eyelids, known as blepharitis, is a common manifestation of ocular rosacea. This can cause redness, swelling, and a gritty or burning sensation.
- Conjunctivitis: Inflammation of the conjunctiva, the clear tissue covering the white part of the eye, may occur. This can lead to redness, tearing, and a feeling of dryness.
- Photophobia: Increased sensitivity to light (photophobia) is another common symptom of ocular rosacea.
- Corneal Involvement: In severe cases, ocular rosacea can lead to corneal involvement, causing corneal damage and vision problems.
- Fluctuating Symptoms: Symptoms of ocular rosacea can be intermittent, with flare-ups and periods of remission. Triggers for flare-ups may include stress, sunlight, or spicy foods.
- Association with Skin Symptoms: Ocular rosacea is often associated with skin symptoms of rosacea, such as facial redness, flushing, and papules/pustules.
- Diagnosis and Treatment: Ocular rosacea is diagnosed by an eye care professional, typically an ophthalmologist. Treatment may involve artificial tears, warm compresses, and eyelid hygiene to manage symptoms. In some cases, oral antibiotics or other medications may be prescribed.
- Long-Term Management: Long-term management of ocular rosacea may include ongoing care from both dermatologists and eye care professionals. Regular eye examinations are essential to monitor for any changes and adjust the treatment plan as needed.
- Lifestyle Modifications: Avoiding triggers, such as sunlight, wind, and environmental irritants, can help manage ocular rosacea symptoms. Additionally, wearing sunglasses with UV protection and practicing good eyelid hygiene are recommended.

Here some common Treatment are:-
- Topical Medications:(i)Metronidazole: This antibiotic gel or cream can help reduce inflammation.(ii)Azelaic Acid: It helps to reduce redness and inflammation and is available in gel or cream form.(iii)Ivermectin: This topical cream can be used to reduce the inflammation associated with rosacea.
- Oral Antibiotics: Doxycycline, Tetracycline, Minocycline: Antibiotics can be prescribed to reduce inflammation. They are often used in low doses for an extended period.
- Oral Acne Medications:
- Isotretinoin: In severe cases, isotretinoin, commonly used for acne, may be prescribed to reduce oil gland activity.
- Topical Steroids (Short-term): Hydrocortisone cream: In some cases, short-term use of mild topical steroids may help with inflammation, but prolonged use can worsen symptoms.
- Laser Therapy: Intense Pulsed Light (IPL) Therapy: This can help reduce redness and the appearance of blood vessels.Laser Therapy: Certain lasers can target blood vessels, reducing their visibility.
- Oral Medications for Severe Cases: Isotretinoin (Accutane): Reserved for severe cases that don’t respond well to other treatments. It has potential side effects and requires careful monitoring.
- Avoid Triggers: Identifying and avoiding triggers, such as spicy foods, alcohol, and extreme temperatures, can help manage symptoms.
- Skincare Routine: Using gentle skincare products and avoiding harsh chemicals can prevent irritation.