Introduction to Abdominal or Thoracic Aortic Aneurysm Surgery
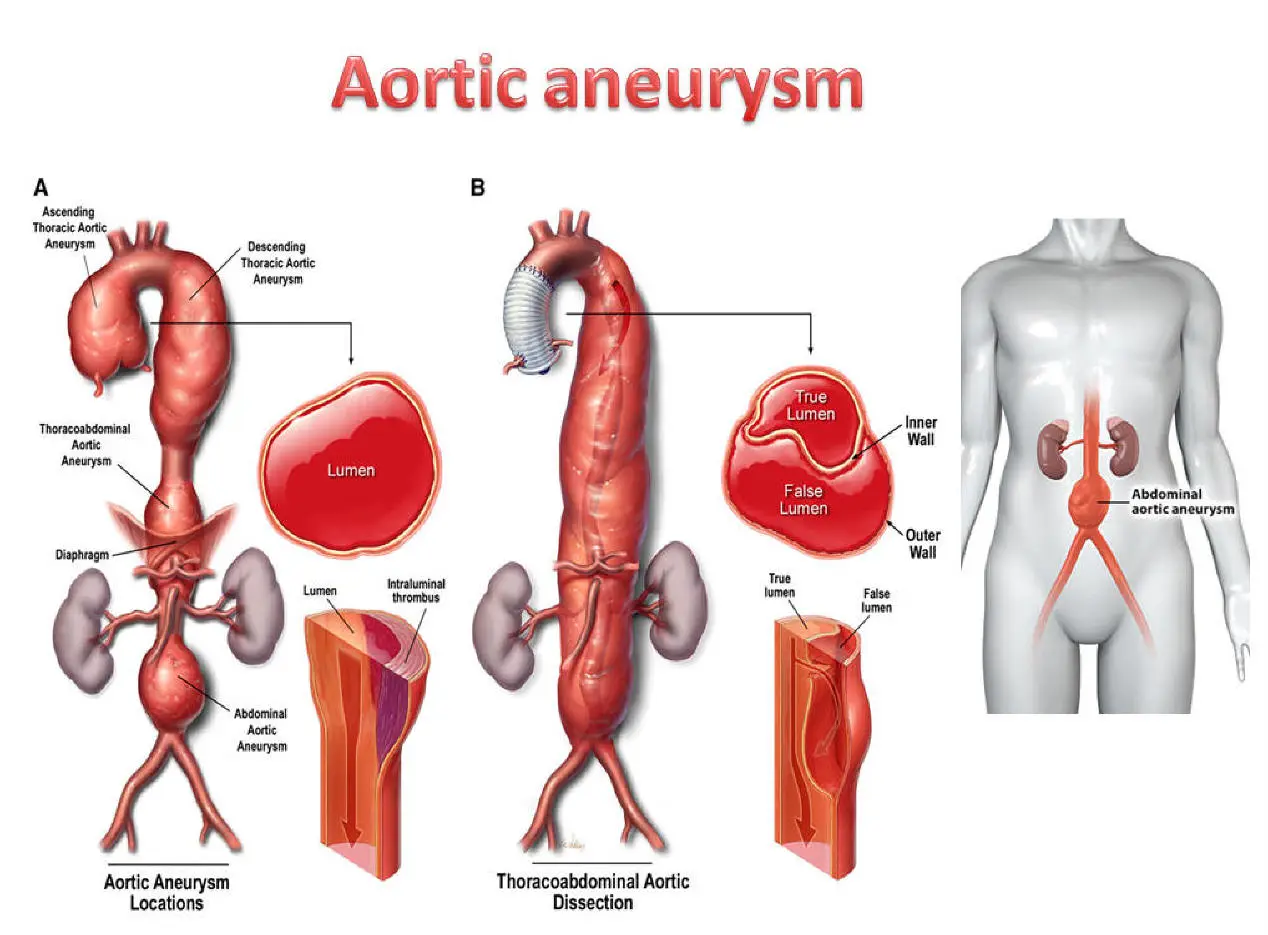
The aorta is the major artery that carries oxygenated blood from the heart to the rest of the body. Over time, due to weakening of its wall (by factors such as hypertension, atherosclerosis, genetic conditions), portions of the aorta may dilate abnormally, forming an aortic aneurysm. When such dilation occurs in the abdominal portion, it's called an abdominal aortic aneurysm (AAA); when in the chest (thoracic aorta), it's a thoracic aortic aneurysm (TAA).
Left untreated, large aneurysms may dissect (a tear in the aortic wall) or rupture, both of which are life-threatening emergencies. Surgical repair of an aortic aneurysm-whether open or endovascular-is aimed at preventing rupture and restoring the integrity of blood flow.
Aneurysm surgery can be broadly categorized into open surgical repair and endovascular (minimally invasive) repair. The choice depends on aneurysm location, size, anatomy, patient comorbidities, and surgical expertise.
In this article, we will delve into the causes, symptoms, diagnosis, treatment options, prevention, complications, and life after surgery for abdominal or thoracic aortic aneurysm repair.
Causes and Risk of Aortic Aneurysm (Abdominal / Thoracic)
Aortic aneurysms-whether abdominal (AAA) or thoracic (TAA)-develop from weakening of the aortic wall due to a combination of genetic, lifestyle, and medical factors. The risks and causes overlap but vary somewhat depending on the aneurysm's location.
Pathophysiology
-
The aortic wall is composed of three layers (intima, media, adventitia). Degeneration of the media (elastic and smooth muscle components) reduces the tensile strength of the wall.
-
Matrix metalloproteinases (MMPs) and other proteolytic enzymes degrade elastin and collagen, sometimes triggered by inflammation, oxidative stress, or mechanical stress.
-
Hemodynamic forces (blood pressure, pulsatile flow) further stress the weakened wall, facilitating progressive dilation.
-
In some genetic/connective tissue disorders (e.g., Marfan syndrome, Ehlers-Danlos, bicuspid aortic valve), structural defects in the aortic wall predispose to aneurysm formation.
Risk Factors
-
Age: Incidence increases with age (especially > 60 years)
-
Sex: Males are more commonly affected (especially for abdominal aneurysm)
-
Hypertension: Elevated arterial pressure accelerates stress on the aortic wall
-
Smoking: Strongly associated with aneurysm formation and expansion
-
Atherosclerosis / Vascular disease: Atherosclerotic changes in the aortic wall promote weakening
-
Family history / genetics: First-degree relatives of patients with aneurysm have higher risk
-
Connective tissue disorders: Marfan, Ehlers-Danlos, Loeys-Dietz syndromes
-
Inflammation / infections: Rarely, mycotic (infectious) aneurysms can weaken the vessel wall
-
Other risk contributors: Hyperlipidemia, chronic kidney disease, chronic smoking, certain inflammatory disorders
Because aneurysms often grow slowly and silently, patients may be asymptomatic until late or until rupture.
Symptoms and Signs of Aortic Aneurysm
Aortic aneurysms often develop silently, with few or no symptoms until they become large or rupture-a medical emergency. The signs and symptoms differ slightly between abdominal (AAA) and thoracic (TAA) aortic aneurysms, but both can present with non-specific pain and alarming features if they rupture or dissect.
Possible Signs & Symptoms (before rupture or dissection)
Abdominal Aortic Aneurysm (AAA):
-
Deep, gnawing abdominal or back pain
-
A pulsatile abdominal mass (if superficial and large enough)
-
Pain radiating to the flank, groin, or legs
-
Feeling of fullness or early satiety
-
Occasionally, embolic phenomena: small clots from the aneurysm sac travel distally, causing limb ischemia, renal infarcts, etc.
Thoracic Aortic Aneurysm (TAA):
-
Chest pain or back pain (especially between the shoulder blades)
-
Cough, hoarseness, or dysphagia (if aneurysm compresses airway or esophagus)
-
Shortness of breath
-
In some cases, signs of aortic root dilation (aortic regurgitation) - murmur of AR
-
Superior vena cava syndrome (rare, if pressing on venous structures)
Emergency Presentation (Rupture or Dissection)
-
Sudden, severe, tearing chest or back pain
-
Hypotension, shock
-
Pulsatile bleeding into thorax or abdomen
-
Loss of consciousness
-
In case of dissection, signs of organ ischemia (stroke, kidney failure, limb ischemia)
Because rupture has extremely high mortality, early detection and timely repair are critical.
Diagnosis of Aortic Aneurysm
Diagnosis of aortic aneurysm-abdominal (AAA) or thoracic (TAA)-relies heavily on imaging, since most aneurysms are asymptomatic and found incidentally or during targeted screening. Physical examination and risk factor assessment are important, but imaging studies are the gold standard for confirmation, sizing, and monitoring.
Physical Examination
-
In AAA, palpation of the abdomen may reveal a pulsatile mass (especially in thin patients)
-
Bruit over the aneurysm
-
However, many aneurysms (especially small or deep) are not felt on exam.
Imaging Modalities
-
Ultrasound (Abdominal US):
-
First-line screening tool for abdominal aneurysms
-
Non-invasive, low cost, no radiation
-
Good sensitivity/specificity for detecting aneurysm and measuring maximal diameter
-
Limited in obese patients or with bowel gas
-
-
Computed Tomography Angiography (CTA):
-
Gold standard for planning surgical or endovascular repair
-
Provides detailed 3D anatomy, branch vessel involvement, neck morphology, and relation to adjacent structures
-
Helps assess suitability for endovascular repair
-
In emergency (rupture), CTA helps localize leak, retroperitoneal bleeding
-
-
Magnetic Resonance Angiography (MRA):
-
Alternative in patients with contrast allergy or renal impairment (if possible)
-
Excellent spatial resolution
-
Longer acquisition time, less available in emergencies
-
-
Conventional Angiography / Digital Subtraction Angiography (DSA):
-
Rarely used primarily now; sometimes used intraoperatively or in complex cases
-
Provides dynamic flow information and access route mapping
-
-
Transesophageal Echocardiography (TEE):
-
Useful for thoracic aneurysms or dissections (intraoperatively)
-
Bedside in emergencies
-
-
Chest / Abdominal X-rays:
-
May incidentally show calcified aortic wall or widened mediastinum
-
Low sensitivity
-
Monitoring & Surveillance
Once an aneurysm is discovered, regular imaging follow-up is needed to monitor growth rate, morphology changes, and guide the timing of repair. For example, small aneurysms (< 4.0 cm) may be followed with ultrasounds or CT scans periodically.
Criteria for Intervention
Deciding when to intervene (i.e. surgical repair) depends on balancing rupture risk vs surgical risk. Some generally accepted thresholds:
-
Abdominal aneurysm: diameter ≥ 5.5 cm in men, ≥ 5.0 cm in women (though local practice may vary)
-
Rapid expansion (e.g. > 0.5 cm growth in 6 months)
-
Symptomatic aneurysm (pain, tenderness)
-
Evidence of impending rupture (e.g., leak, wall contrast enhancement)
-
Branch involvement or risk to visceral or renal arteries
The European and American vascular surgery societies publish guidelines (for example, the 2024 ESVS guidelines) to guide decision thresholds.
Treatment Options for Abdominal or Thoracic Aortic Aneurysm Surgery
Once the decision for repair is made, surgeons typically choose between open surgical repair and endovascular repair. In some complex thoracoabdominal aneurysms, hybrid approaches are used.
Open Surgical Repair (Conventional)
Procedure:
-
The surgeon gains direct access via a large incision (abdominal, thoracic, or thoracoabdominal).
-
The aorta is clamped above and below the aneurysm (stop blood flow temporarily).
-
The diseased (dilated) segment is removed (or excluded) and replaced with a synthetic graft (e.g. Dacron tube or bifurcated graft).
-
Branch arteries, renal arteries, visceral arteries are reattached or incorporated, depending on location (in thoracoabdominal).
-
After completion, clamps are released gradually, and blood flow restores.
Pros & Cons:
-
Pros: durable, long-term patency, fewer late reinterventions
-
Cons: large incision, higher perioperative morbidity, longer recovery time, greater physiologic stress
This is still considered the "standard" in many settings, especially when anatomy is unsuitable for endovascular options.
Endovascular Repair (Minimally Invasive) - EVAR / TEVAR / Branched Devices
Definitions:
-
EVAR (Endovascular Aneurysm Repair) - for abdominal aorta
-
TEVAR (Thoracic Endovascular Aortic Repair) - for thoracic aortic aneurysm
-
Branched / Fenestrated Endografts / Hybrid - for complex cases involving visceral branches or aortic arch
Procedure:
-
Under imaging guidance (fluoroscopy), a delivery system is introduced percutaneously (via femoral or iliac arteries) or via small surgical cutdowns.
-
A stent-graft (device composed of fabric with metallic stents) is navigated to the aneurysm and deployed, creating a new lumen, excluding the aneurysm sac.
-
The aneurysm sac thromboses over time, and pressure on the wall is relieved.
-
If the aneurysm involves arterial branches (renal, mesenteric, spinal), more complex techniques like fenestrated or branched stent grafts are used, or hybrid approach combining surgical bypass and endograft.
Advantages & Limitations:
-
Advantages: lower immediate mortality, less invasive, shorter hospital stay, quicker recovery
-
Limitations: not all aneurysms are anatomically suitable (short necks, tortuosity, branch involvement), higher rates of re-intervention (e.g., endoleaks)
-
Surveillance is mandatory after EVAR to detect complications (endoleaks, migration)
-
For thoracoabdominal aneurysms, risk of spinal cord ischemia is a concern, especially with extensive stent coverage.
Hybrid Techniques / Adjuncts
-
Sometimes surgeons perform open surgical bypass of certain branch arteries (e.g. visceral) and then deploy an endograft for the rest ("hybrid repair").
-
Fenestrated or branched stent grafts are custom designed with openings (fenestrations) matching branch vessel origins.
-
In some thoracic cases, valve-sparing root replacement or Bentall procedure may be needed if the root or aortic valve is involved.
Emergency Repair
If a rupture or dissection occurs, emergent open or endovascular repair is performed as a lifesaving procedure. Mortality is much higher in emergent settings.
Postoperative Care & Monitoring
-
Intensive care monitoring (hemodynamics, renal function, bleeding)
-
Imaging (CT angiography) before discharge to confirm graft positioning and absence of leaks
-
Antihypertensive control, anticoagulation or antiplatelet therapy (as per surgeon's protocol)
-
Long-term surveillance imaging (CTA/MRA periodically) to detect graft integrity or complications
Outcomes & Survival
-
Elective open repair survival is quite favorable (survival rates 95-98%) when no rupture occurs.
-
For ruptured aneurysms, survival is much lower (50-70 %) despite repair.
-
EVAR offers lower perioperative mortality but may require more reinterventions in the longer term.
Prevention and Management (Before After Surgery)
Prevention and management of aortic aneurysm-both before and after surgery-focus on risk factor reduction, patient optimization, and careful medical or surgical follow-up. Thoughtful care lowers rupture risk, improves surgical outcomes, and supports recovery.
Prevention / Risk Reduction (Primary & Secondary)
Because surgery treats the structural problem, prevention addresses modifiable risk factors:
-
Quit smoking (mandatory)
-
Strict blood pressure control (especially systolic <130 mmHg)
-
Lipid management / statins
-
Lifestyle changes: diet, weight control, regular exercise (within cardiovascular tolerance)
-
Control comorbidities: diabetes, chronic kidney disease
-
Periodic screening / surveillance in high-risk populations (e.g. men >65 with smoking history)
-
Family screening if first-degree relative has aneurysm
Even after surgery, these measures remain vital to prevent disease in other vascular beds and preserve graft and vascular health.
Preoperative Optimization
-
Cardiovascular risk assessment (ECG, echocardiography, coronary evaluation)
-
Pulmonary function tests, renal function, and other comorbid evaluation
-
Nutritional support, smoking cessation ahead of surgery
-
Pre-surgery imaging planning and sizing
Postoperative Management & Long-term Follow-up
-
Careful blood pressure control (often with beta-blockers, ACE inhibitors)
-
Antiplatelet therapy (as per vascular surgeon / cardiologist)
-
Lipid-lowering therapy
-
Regular imaging follow-up (e.g., CTA/MRA annually or as recommended)
-
Monitor for graft complications (e.g. endoleaks, graft migration, branch stenosis)
-
Gradual return to physical activity under guidance
-
Lifestyle counseling and vascular risk factor management
Complications of Aortic Aneurysm Surgery
Aortic aneurysm surgery-whether open or endovascular-carries risks of serious complications, though most are rare when the procedure is planned and performed by experienced teams. These complications can involve multiple organs, and some may be life-threatening or require further intervention.
Perioperative / Early Complications
-
Bleeding / hemorrhage
-
Renal failure / acute kidney injury (from contrast, hypoperfusion)
-
Cardiac complications: myocardial infarction, arrhythmia
-
Respiratory complications: pneumonia, atelectasis, prolonged ventilation
-
Infection: graft infection, wound infection
-
Ischemic injury / organ dysfunction (especially intestines)
-
Spinal cord ischemia / paralysis (especially in thoracic / thoracoabdominal repairs)
-
Stroke / neurological deficit
-
Graft thrombosis or occlusion
-
Endoleaks (in EVAR): persistent blood flow into the aneurysm sac
-
Graft migration, kinking, fabric failure
-
Distal embolization (embolus traveling to limbs or organs)
-
Reoperation or need for secondary interventions
Late Complications
-
Endoleaks (type I, II, III, IV, V) and sac expansion
-
Graft degeneration or fatigue
-
Branch vessel stenosis or occlusion (renal, mesenteric arteries)
-
Aortoenteric or aortocaval fistula formation
-
Late graft infection
-
Pseudoaneurysm formation at anastomotic sites
-
Recurrent aneurysm or new aneurysm formation in other aortic segments
-
Chronic pain or graft-related discomfort
Surveillance and timely detection of complications are essential.
Living with the Condition / Post-Surgery Life
Life after aortic aneurysm surgery usually involves a period of healing, gradual return to daily activities, and ongoing focus on cardiovascular health and risk reduction. Most patients experience a dramatic improvement in life expectancy and quality if recovery guidance is followed, but adjustments and regular monitoring are essential.
Recovery Phase
-
Hospital stay ranges 5-10 days or more (longer for open surgery)
-
Rehabilitation and physical therapy to regain strength
-
Gradual reintroduction of daily activities (avoiding lifting, strenuous exertion early)
-
Monitoring wound healing, renal function, hemodynamics
-
Pain control and psychological support
Long-Term Follow-up
-
Lifelong imaging follow-up (typically CTA or MRA periodically) to monitor graft and detect complications
-
Strict risk factor control (BP, lipids, smoking)
-
Regular cardiovascular follow-up
-
Prompt reporting of symptoms such as new pain, limb weakness, abdominal discomfort, or signs of ischemia
-
Possibly lifelong antiplatelet therapy or anticoagulation (depending on graft or concomitant conditions)
Lifestyle and Functional Outcomes
-
Many patients return to normal daily activities, though heavy exertion may be limited
-
More cautious approach to high-impact sports
-
Diet, weight control, and exercise (as tolerated) remain crucial
-
Psychological adjustment: patients may feel anxiety about recurrence or graft integrity
-
Education and awareness: patients should carry records of graft type, imaging history, and treat providers as partners in surveillance
Prognosis
-
Elective repairs in non-ruptured aneurysms have excellent prognosis when well managed
-
With proper follow-up and control of comorbidities, many patients live decades after repair
-
Some risk remains for additional vascular disease; hence, lifelong care is needed
Top 10 Frequently Asked Questions about Abdominal or Thoracic Aortic Aneurysm Surgery
1. What is an aortic aneurysm, and how does it develop?
An aortic aneurysm is an abnormal bulging or ballooning of the wall of
the aorta - the body's main artery that carries blood from the heart to the rest of the
body.
It can occur in two main areas:
-
Abdominal Aortic Aneurysm (AAA): In the lower part of the aorta, in the abdomen.
-
Thoracic Aortic Aneurysm (TAA): In the chest portion of the aorta.
Aneurysms usually develop due to weakening of the artery wall, caused by factors such as high blood pressure, smoking, aging, genetic conditions (like Marfan or Ehlers-Danlos syndrome), or atherosclerosis (plaque buildup).
2. What are the symptoms of an abdominal or thoracic aortic aneurysm?
In many cases, aortic aneurysms cause no symptoms and are discovered incidentally during imaging tests. However, as they enlarge or rupture, symptoms may include:
-
For Abdominal Aneurysm: Deep, persistent pain in the abdomen or lower back, pulsating sensation near the navel.
-
For Thoracic Aneurysm: Chest or upper back pain, shortness of breath, difficulty swallowing or coughing.
A ruptured aneurysm is a life-threatening emergency and requires immediate surgery.
3. When is surgery recommended for an aortic aneurysm?
Surgery is usually recommended when:
-
The aneurysm reaches a critical size (≥5.5 cm for abdominal, ≥6.0 cm for thoracic).
-
The aneurysm is growing rapidly (more than 0.5 cm in 6 months).
-
There are symptoms such as pain, pressure, or signs of rupture.
-
There's a risk of rupture due to genetic or structural abnormalities.
Your vascular surgeon will determine the best timing for surgery based on size, location, growth rate, and overall health.
4. What are the main types of aortic aneurysm surgery?
There are two primary surgical approaches:
-
Open Surgical Repair (OSR):
-
The surgeon makes a large incision in the chest or abdomen to replace the weakened section of the aorta with a synthetic graft (tube).
-
Typically used for large or complex aneurysms.
-
-
Endovascular Aneurysm Repair (EVAR/TEVAR):
-
A minimally invasive procedure where a stent graft is inserted through small incisions in the groin and guided to the aneurysm site via blood vessels.
-
Commonly used for patients at higher surgical risk or those with suitable anatomy.
-
Your surgeon will choose the most appropriate method based on the aneurysm's location and your health condition.
5. What is the difference between abdominal and thoracic aortic aneurysm surgery?
The main difference lies in the location of the aneurysm and the surgical approach:
-
Abdominal Aortic Aneurysm (AAA) Surgery: Involves the aorta in the lower abdomen. It can be done using open repair or EVAR (Endovascular Aneurysm Repair).
-
Thoracic Aortic Aneurysm (TAA) Surgery: Involves the aorta in the chest. It requires thoracotomy (chest incision) for open repair or TEVAR (Thoracic Endovascular Aneurysm Repair) for minimally invasive repair.
Recovery and risk factors differ slightly depending on which section of the aorta is affected.
6. What are the risks and complications associated with aortic aneurysm surgery?
Although both open and endovascular aneurysm repairs are generally safe, there are potential risks, including:
-
Bleeding or infection
-
Heart or lung complications
-
Kidney injury
-
Graft leakage (in EVAR/TEVAR)
-
Blood clots or stroke
-
Spinal cord injury (rare, in thoracic repairs)
Careful preoperative evaluation and postoperative monitoring help minimize these risks.
7. How long does recovery take after aortic aneurysm surgery?
-
Open surgery: Hospital stay typically lasts 7-10 days, with full recovery taking about 6-12 weeks.
-
Endovascular (EVAR/TEVAR): Hospital stay is shorter (2-4 days) with recovery in 2-3 weeks.
Recovery time depends on your age, overall health, and the complexity of the procedure. Regular follow-up scans are required to monitor graft stability.
8. What lifestyle changes are recommended after aortic aneurysm surgery?
Post-surgery, maintaining heart and blood vessel health is crucial. Doctors recommend:
-
Quit smoking permanently.
-
Control blood pressure and cholesterol levels with medication and diet.
-
Eat a heart-healthy diet rich in fruits, vegetables, lean proteins, and whole grains.
-
Exercise regularly, but avoid heavy lifting or straining.
-
Attend follow-up appointments and imaging scans as scheduled.
These changes help prevent new aneurysms and promote long-term vascular health.
9. What happens if an aortic aneurysm is left untreated?
If left untreated, an aortic aneurysm can continue to enlarge, eventually leading to
rupture or dissection (tearing of the aortic wall).
A rupture causes severe internal bleeding and is often fatal within
minutes if not treated immediately.
Early diagnosis and timely surgical intervention dramatically improve survival and
quality of life.
10. What is the long-term outlook after aortic aneurysm surgery?
The prognosis after aneurysm surgery is generally very good, especially with early detection and proper management.
-
Open repair: The graft is durable and can last a lifetime.
-
Endovascular repair (EVAR/TEVAR): Regular monitoring via imaging (CT scans or ultrasounds) is necessary to check for graft leaks or movement.
Most patients can return to normal activities and enjoy an active, healthy life after full recovery.


