Introduction to Ankle Replacement
The ankle joint bears tremendous loads, facilitates complex motions (dorsiflexion, plantarflexion, inversion, eversion), and plays a critical role in gait, balance, and mobility. When the ankle is severely diseased or degenerated—often due to osteoarthritis or prior trauma—pain, stiffness, deformity, and functional limitation can profoundly affect quality of life.
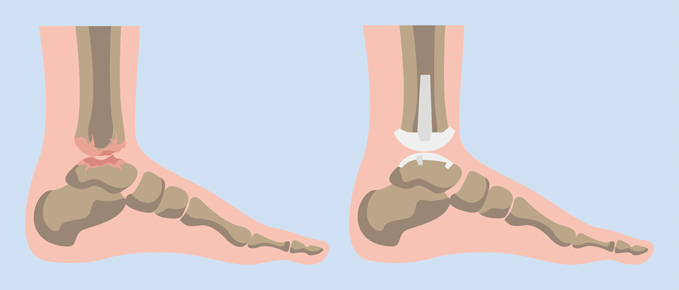
While ankle fusion (arthrodesis) has historically been the standard surgical remedy, it eliminates joint motion and increases stress on adjacent joints. Over the past few decades, total ankle replacement (TAA) has evolved as an alternative, aiming to relieve pain while preserving motion and more physiologic biomechanics. Advances in implant designs, surgical techniques, patient selection, and rehabilitation have significantly improved outcomes and expanded indications.
In this guide, we explore:
-
Causes and risk factors underlying ankle conditions that lead to replacement
-
Clinical signs and symptoms
-
Diagnostic workup and candidacy evaluation
-
Treatment options and surgical techniques
-
Pre- and post-op management
-
Risks, complications, and failure modes
-
Long-term care, patient expectations, and living with a replaced ankle
Causes, Indications Risk Factors (Why Ankle Replacement Is Needed)
An ankle replacement (total ankle arthroplasty) becomes necessary when severe arthritis or trauma causes persistent pain, stiffness, and loss of movement that cannot be managed by medication, physical therapy, or assistive devices. The procedure replaces the damaged parts of the ankle joint with artificial implants to restore motion and reduce pain.
1. Underlying Pathologies / Indications
Ankle replacement is a treatment, not a disease. It is indicated in end-stage ankle joint disease when conservative treatments fail. Common underlying causes include:
-
Primary (idiopathic) osteoarthritis of the ankle (though less common than in knee/hip)
-
Post-traumatic arthritis: fractures, malunions, ligament injuries, instability, cartilage damage after injury
-
Inflammatory arthritis: rheumatoid arthritis or other autoimmune arthritides
-
Osteonecrosis / avascular necrosis of the talus or tibial plafond
-
Failed prior ankle surgeries or hardware complications
-
Deformity or malalignment (varus/valgus tilt) contributing to joint load imbalance
-
Adjacent joint degeneration worsening the overall foot-ankle complex
The decision toward TAA is often made when the patient has disabling pain, loss of function, and inadequate relief with non-surgical measures.
The American Orthopaedic Foot & Ankle Society (AOFAS) position suggests that before TAA is considered, patients should have exhausted conservative therapy, have adequate vascular status, and a suitable soft-tissue envelope around the ankle to permit safe surgery.
2. Risk Factors, Patient Traits, and Contraindications
While many patients may seem candidates, success depends on careful selection. Risk factors and contraindications include:
Risk Factors / Less Ideal Traits
-
Younger age (< 55 years): Younger patients tend to have higher demands and higher long-term stress on implants; in large cohort studies, younger age was an independent risk for TAA failure.
-
Poor bone quality or osteoporosis: Insufficient bone stock or weak subchondral bone can impair fixation or lead to subsidence
-
Severe deformity or malalignment that cannot be corrected intraoperatively
-
Soft tissue compromise: prior trauma, scars, poor vascularity, skin ulcers
-
Active or prior infection in the ankle or adjacent bones
-
Severe instability / ligament insufficiency that cannot be managed
-
Peripheral vascular disease, poor circulation, neuropathy
-
Obesity or high body mass index (BMI): Some recent evidence suggests higher BMI may correlate with worse outcomes or complications.
-
Unwillingness / inability to adhere to rehabilitation or activity restrictions
-
Charcot arthropathy (in many cases): Because of neuropathy and bone destruction, replacement often fails in poorly controlled neuropathic joints
Contraindications (Absolute / Relative)
-
Active infection in or near the joint
-
Severe bone loss or structural insufficiency
-
Uncorrectable deformity
-
Inadequate soft-tissue coverage or vascular supply
-
Neuropathic destruction with uncontrolled progression
-
Severe medical comorbidities or poor healing potential
Importantly, TAA may require adjunct procedures (osteotomies, ligament reconstructions, realignment) in many patients to optimize alignment and stability.
Modern implant designs, surgical planning, and patient-specific instrumentation (PSI) or navigation are helping expand candidacy boundaries.
Symptoms and Signs Acupressure Treats
Acupressure is a traditional healing technique that helps relieve various symptoms and signs by stimulating the body's natural self-healing mechanisms through pressure applied to specific points. It is often used as a complementary therapy to balance energy flow (Qi), reduce pain, and relieve stress-related conditions rather than serving as a direct treatment for structural diseases.
Common Conditions Treated by Acupressure
Acupressure is highly effective in addressing a broad range of physical and emotional symptoms. Some of the most common symptoms acupressure can treat include:
-
Pain:
-
Chronic pain conditions like neck pain, back pain, joint pain, and muscle soreness can benefit from acupressure techniques. Common acupoints like LI4 (located between the thumb and index finger) are widely used for general pain relief.
-
-
Stress and Anxiety:
-
Acupressure targets specific points that help calm the nervous system, lower blood pressure, and alleviate feelings of anxiety. Regular acupressure can significantly reduce stress and improve mental clarity.
-
-
Headaches:
-
Acupressure can help reduce the severity and frequency of headaches and migraines by applying pressure to points like Yintang (the point between the eyebrows), GB20 (at the base of the skull), and LI4.
-
-
Sleep Disorders:
-
Individuals who suffer from insomnia or restless sleep can benefit from acupressure to improve sleep quality and promote relaxation, helping them fall asleep more easily.
-
-
Digestive Issues:
-
Nausea, bloating, indigestion, and constipation are common ailments that can be addressed with acupressure. For example, P6 (Neiguan) is a well-known acupoint used for nausea relief, particularly for motion sickness or during chemotherapy.
-
Diagnosis, Evaluation Pre-operative Workup
Diagnosis and pre-operative workup for ankle replacement surgery involve a careful evaluation of joint condition, patient health status, and surgical planning to ensure optimal outcomes. These steps identify the degree of arthritis, rule out infection or deformity, and guide prosthesis selection and placement.
1. History & Physical Examination
-
Detailed onset / duration / progression of symptoms
-
Past history: trauma, surgeries, fractures, injections, deformities
-
Prior treatments: medications, orthotics, braces, physiotherapy
-
Comorbidities: diabetes, vascular disease, smoking, osteoporosis, neuropathy
-
Functional limitations, activity goals, expectations
-
Vascular status: pulses, capillary refill, ankle-brachial index (ABI)
-
Skin condition, scars, prior incisions
-
Gait assessment
-
Physical exam: alignment, swelling, tenderness, range-of-motion, ligament stability, foot/ankle adjacent joint mobility
2. Imaging & Radiographic Workup
-
Plain radiographs (weight-bearing):
AP (anteroposterior) view
Lateral view
Oblique / mortise views
Evaluate joint space narrowing, osteophytes, subchondral sclerosis, bone cysts, deformities, alignment
Hindfoot alignment films or long leg alignment (when needed) -
CT scan: for bony morphology, bone stock, cysts, deformity, trial templating
-
MRI: helpful to assess soft tissue structures (ligaments, tendons, synovium, cartilage, bone marrow edema)
-
Bone scan or SPECT-CT (in selected cases): to detect occult infection or bone activity
-
Dynamic / stress views: to assess alignment under load
-
Pre-op templating / planning: crucial for component sizing, orientation, and anticipated corrections
3. Laboratory & Medical Workup
-
CBC, ESR, CRP (to screen for inflammation or occult infection)
-
Renal function, electrolytes
-
Metabolic panels, vitamin D, bone markers
-
HbA1c / glucose, lipid profile
-
Vascular studies if indicated
-
Preoperative anesthesia clearance (ECG, chest X-ray, cardiac risk)
-
If prior hardware or suspicion of infection: aspiration / cultures
4. Preoperative Planning & Decisions
-
Patient counseling and expectation management: explain risks, rehabilitation, realistic outcomes
-
Assessment of alignment and correction needs
-
Planning adjunct procedures: such as osteotomies (e.g. tibial or fibular), ligament balancing, soft-tissue releases, hindfoot corrections
-
Selection of implant design (fixed-bearing vs mobile-bearing, stemmed vs non-stemmed) and instrumentation
-
Risk stratification and optimization: smoking cessation, control of diabetes/vascular disease, improve bone health
In essence, the success of TAA hinges not just on implant selection, but on meticulous pre-operative planning, soft tissue balance, alignment correction, and patient optimization.
Treatment Options Surgical Techniques
Treatment options and surgical techniques for advanced ankle arthritis primarily include total ankle replacement (arthroplasty) and ankle fusion (arthrodesis). Alternatives such as minimally invasive procedures, tendon or ligament repairs, and soft tissue reconstructions may be chosen based on individual patient factors.
1. Conservative / Non-surgical Treatments (Before TAA)
Most patients will undergo a spectrum of nonoperative approaches before considering replacement:
-
Analgesics / NSAIDs / pain modulation
-
Activity modification / rest / offloading
-
Bracing / ankle-foot orthoses (AFOs), custom orthotics
-
Physical therapy: strengthening, stretching, mobilization, balance training
-
Injections: corticosteroids, hyaluronic acid, platelet-rich plasma (PRP) (evidence is mixed)
-
Joint distraction (in specialized centers)
-
Arthroscopic debridement / osteophyte removal (in milder disease)
-
Realignment (osteotomies) or ligamentous surgery if deformity or instability contribute significantly
When these fail to relieve pain and restore function, and the patient is a suitable candidate, TAA is considered.
2. Surgical Techniques & Implant Types
Historical Context & Evolution
-
Early ankle replacements (1970s onward) had high failure rates; over time, designs evolved through multiple generations, achieving better outcomes.
-
Newer designs focus on better kinematics, smaller bone resection, and more forgiving fixation strategies.
Implant Types & Design Considerations
-
Fixed-bearing designs: the bearing surface (usually polyethylene) is fixed between tibial and talar components
-
Mobile-bearing (or three-component) designs: the bearing element can move, theoretically reducing edge stresses
-
Cemented vs Cementless (press-fit) fixation
-
Stemmed vs Non-stemmed components
-
Patient-specific instrumentation or custom implants / PSI
-
Navigation or robotic-assisted implantation are being explored in some centers
-
Biomechanical goals: reproduce natural ankle kinematics, maintain congruity through range of motion, minimize shear stress, avoid edge loading.
Surgical Approaches & Techniques
The choice of surgical approach has implications for soft tissues, healing, complications, and ease of component insertion.
-
Anterior approach: classic approach, good access to tibial and talar surfaces, but risk of wound-healing complications, particularly in patients with tenuous soft tissues. Some reports note higher wound complication risk with this route.
-
Lateral (or lateral transfibular) approach: provides alternate access, potentially better component alignment, but may risk fibular complications, nonunion, or additions.
-
Surgeons choose based on patient anatomy, prior scars, bone deformities, soft tissue status, and their own familiarity.
Surgical Steps (generalized):
-
Anesthesia & Positioning: regional or general anesthesia; supine or slight flexion
-
Incision & Exposure: carefully dissecting through skin, soft tissues, preserving vascular supply
-
Bone cuts / resection: remove distal tibial and proximal talar arthritic surfaces, prepare bone beds for implantation
-
Trialing & soft tissue balancing: trials inserted, alignment and ligament balance assessed
-
Implant insertion / fixation: final components placed (with or without cement)
-
Bearing insertion (fixed or mobile component)
-
Alignment correction and adjunct procedures: fibular osteotomies, osteotomies, ligament reconstructions, patency of peritalar structures
-
Closure & soft tissue management: layered closure, drains if needed, ensure coverage
-
Immobilization / early protection: apply splints, boots, or casts
-
Immediate post-op imaging: confirm component placement, alignment, and absence of malposition
Post-op protocols vary by surgeon and implant, but gradual rehabilitation is essential.
3. Rehabilitation & Post-operative Care
A well-structured rehabilitation program is critical to success.
Early Phase (0-2 weeks)
-
Immobilization (splint, cast, boot)
-
Elevation, icing, edema control
-
Pain control, DVT prophylaxis
-
Non-weight-bearing (strict), sometimes toe-touch permitted
Intermediate Phase (Weeks 2-6)
-
Begin passive and gentle active assisted range-of-motion exercises (as allowed)
-
Soft tissue mobilization, gentle stretching
-
Isometric strengthening of surrounding muscles
-
Continue non-weight-bearing or limited weight as per surgeon's protocol
Advanced Phase (Weeks 6-12)
-
Gradual weight-bearing in controlled manner (boot or walking frame)
-
Gait training
-
Progressive strengthening and proprioceptive training
-
Balance and neuromuscular control
Late Phase (3-6 months onward)
-
Transition to full weight-bearing
-
Increase functional training, low-impact aerobic exercise (walking, cycling, swimming)
-
Gradual return to daily-life activities
-
Avoidance of high-impact sports unless explicitly cleared
-
Ongoing monitoring of pain, swelling, function
Outcomes depend heavily on adherence, quality of therapy, and appropriate progression of loading.
Prevention, Optimization Management Strategies
Prevention and optimization of ankle arthritis—along with management strategies for those recovering from ankle replacement—revolve around early risk factor modification, appropriate conservative management, and best practices before and after surgery. Implementing these steps can drastically slow disease progression and improve surgical outcomes.
1. Pre-operative Optimization & Preventive Strategies
-
Smoking cessation well in advance of surgery
-
Control comorbidities: diabetes, hypertension, vascular disease
-
Bone health optimization: treat osteoporosis, vitamin D supplementation
-
Weight management / obesity reduction
-
Skin and soft tissue evaluation: address ulcers, scars, vascular status
-
Prehabilitation physical therapy to strengthen muscles, improve range-of-motion, and prepare patient
-
Patient education & expectations counseling
-
Nutritional optimization and general fitness
2. Intraoperative & Surgical Measures to Prevent Complications
-
Gentle soft tissue handling
-
Adequate exposure and soft tissue release to avoid tension
-
Precise alignment and balanced ligament tensions
-
Use of drains or appropriate closure techniques
-
Meticulous hemostasis
-
Judicious use of prophylactic antibiotics
-
Use of navigation/PSI to enhance implant positioning
3. Post-operative Surveillance & Early Management
-
Frequent wound checks, careful wound care
-
Early recognition and management of infection
-
DVT prophylaxis per protocol (anticoagulants, compression)
-
Regular imaging (X-rays) at intervals (e.g., 6 weeks, 3 months, 6 months, yearly)
-
Monitor for signs of loosening, subsidence, osteolysis, component migration
-
Prompt intervention if complication signs appear (pain, swelling, instability, radiographic changes)
-
Gradual progression of weight-bearing, with close oversight
Proactive and vigilant post-op care is essential to salvage potential problems early.
Complications, Failure Modes Risk Rates
Complications and failure modes in ankle replacement (total ankle arthroplasty) are more frequent compared to knee or hip replacements, though most patients experience significant pain relief and functional improvement. Key risks, failure modes, and their rates are summarized below.
1. Incidence / Rates from Literature
-
A systematic review across 22 studies (4,412 ankles) found an adjusted mean complication rate of 23.7% (range 2.4% to 52%), with many being high-grade complications.
-
In a large series of 16,964 ankles (127 studies), common pooled complications included intraoperative fracture (6%) and impingement (6%).
-
In 5,619 TAA procedures with population-based data, 5-year survival was 95.4%, 10-year survival was 91.1%. Major complications included wound healing issues, talar collapse, and implant loosening.
-
Early failure analysis of >2,157 TAAs showed that early failures still pose a concern relative to other joint arthroplasties.
-
Older devices had higher reoperation rates; e.g., in one series of second-generation Agility implants, 28% underwent reoperations (127 reoperations in 306 ankles) over ~33 months.
-
Modern implant series report 5-year revision rates of ~4-8% for current generation designs.
These statistics underscore that while TAA has improved, careful patient selection and technique remain critical.
2. Common & Serious Complications
-
Wound-healing problems / soft tissue complications
-
Delayed healing, dehiscence, necrosis, skin breakdown
-
Especially in anterior-approach cases or patients with compromised soft tissues or vascular supply.
-
-
Infection / periprosthetic infection
-
Superficial and deep infections; deep ones may require implant removal or revision
-
Associated with prior infections or poor soft tissues
-
-
Intraoperative fractures / periprosthetic fractures
-
Tibial, talar, or malleolar fractures occurring during bone preparation or manipulation
-
May require fixation, plating, or alteration of implant plan
-
-
Implant loosening / osteolysis / subsidence
-
Gradual loosening of components or sinking into bone
-
Bone loss around implant (osteolysis) due to wear debris or stress shielding
-
-
Component wear, liner fracture, edge loading or impingement
-
Wear of the polyethylene bearing (in both fixed and mobile designs)
-
Fracture or delamination of liner
-
Impingement of components in certain ranges of motion (gutter impingement)
-
Edge loading if alignment is suboptimal
-
-
Malalignment / malposition / instability / mechanical failure
-
Incorrect position, rotation, tilt, or axis imbalance may lead to early failure
-
Instability or subluxation of the implant
-
Mechanical breakage in rare cases
-
-
Talar collapse / bone collapse under component
-
Collapse of the talar subchondral bone under stress, particularly if bone quality is poor
-
-
Adjacent joint overload / progression
-
Though TAA preserves ankle motion, adjacent subtalar or midfoot joints may degenerate over time
-
-
Nerve injury / neurologic complications
-
Injury to superficial or deep peroneal nerves, tibial, saphenous branches
-
Sensory changes, pain, numbness
-
-
Tendon injury / soft tissue impingement
-
Irritation/impingement of surrounding tendons
-
Soft tissue discomfort, bursitis
-
-
Thromboembolism (DVT / PE)
-
Though lower risk than hip/knee arthroplasty, still present
-
-
Need for revision surgery / salvage (fusion conversion)
-
In some cases of failure, removal and conversion to fusion or re-replacement may be required
-
Revision surgery outcomes generally are more guarded
-
Because many of these complications are interrelated (e.g., malalignment increases stress and may accelerate loosening or wear), meticulous surgical technique and post-op surveillance matter.
Living with a Replaced Ankle - Patient Experience, Expectations Long-Term Management
Living with an ankle replacement typically brings substantial pain relief, better mobility, and improved quality of life, though patients should maintain realistic expectations and commit to long-term care. Patient experiences suggest a profound improvement in day-to-day function, with most enjoying activities like walking, cycling, swimming, and light hiking while avoiding high-impact sports.
1. Recovery Timeline & Functional Outcomes
-
Early improvements in pain often occur within weeks to months
-
Functional improvement and plateau usually by 6-12 months, though full maturation can take longer
-
Many patients report excellent satisfaction, improved gait, and enhanced range-of-motion compared to their preoperative state
-
However, residual pain or stiffness is not uncommon: older series reported residual pain in 27%-60% of patients.
-
Implant survival remains promising in modern series (e.g., 91.1% at 10 years) if patient and implant are well-matched.
-
Return-to-sport in low-impact activities (cycling, swimming, dancing) has been documented; return to high-impact sports is generally discouraged or restricted. In a review of anterior vs lateral approach outcomes, return to athletic activity rates of over 60% were reported in select patients.
2. Long-Term Follow-up & Monitoring
-
Scheduled follow-up visits (e.g. 6 weeks, 3 months, 6 months, yearly) with physical exam and imaging
-
Radiographs (AP, lateral) to monitor position, alignment, signs of loosening, subsidence, lucent lines
-
Clinical symptom review: any new or worsening pain, swelling, instability
-
Advanced imaging (CT, SPECT-CT) may be used if loosening or osteolysis is suspected
-
Prompt intervention if complications are detected early (e.g., minor loosening, isolated osteolysis) to preserve the implant
3. Lifestyle Adjustments, Maintenance & Self-Care
-
Maintain healthy body weight to reduce stress on implant
-
Low-impact activities are preferred: walking, stationary cycling, swimming
-
Avoid high-impact sports (running, basketball, jumps) unless surgeon absolutely clears
-
Strengthening, balance & proprioception exercises should continue lifelong
-
Appropriate footwear / orthotics for stability, cushioning, and proper alignment
-
Protect the ankle from trauma or falls — use of supportive braces in risky settings
-
Smoking abstinence, good nutrition, and management of comorbidities (diabetes, vascular disease, bone health)
-
Self-monitoring: any sudden pain, swelling, clicking, instability, or change in function should be evaluated quickly
-
Patient education is key—knowing warning signs, adhering to precautions, and understanding that the implant is not invincible
4. When Revision or Salvage Is Necessary
-
If complications (loosening, infection, component failure) occur, revision TAA or conversion to ankle fusion may be required
-
Success of revisions is more challenging; outcomes depend on bone stock, soft tissues, prior damage, and surgeon expertise
-
In planning revisions, adjacent foot alignment and compensatory joints often must be addressed
5. Quality-of-Life, Expectations & Patient Counseling
-
Realistic expectations are essential: patients should understand that while TAA can reduce pain and improve function, it may not return the ankle to “normal”
-
Emphasize gradual recovery, the importance of rehabilitation, compliance, and lifestyle adjustments
-
Use of patient-reported outcome measures (PROMs) (e.g., ankle-specific scores, general health scores) helps track progress
-
Including patient stories or case vignettes (de-identified) can help illustrate typical journeys, challenges, and outcomes
Top 10 Frequently Asked Questions about Ankle Replacement
1. What is Ankle Replacement Surgery?
Ankle replacement surgery, also known as total ankle arthroplasty, is a surgical procedure in which a damaged ankle joint is replaced with an artificial implant. It is primarily performed to relieve chronic pain, stiffness, and limited mobility caused by severe arthritis or injury.
Unlike ankle fusion, which permanently joins the bones together, ankle replacement preserves joint movement while alleviating pain.
2. Who is a candidate for Ankle Replacement Surgery?
Ideal candidates include individuals who:
-
Suffer from severe ankle arthritis (osteoarthritis, rheumatoid arthritis, or post-traumatic arthritis)
-
Experience chronic pain and stiffness that limit daily activities
-
Have tried non-surgical treatments such as medications, braces, or physical therapy without relief
-
Are in good overall health with adequate bone quality to support the implant
-
Have realistic expectations about post-surgical outcomes
Patients with severe deformities or poor bone quality may be better suited for ankle fusion rather than replacement.
3. How is Ankle Replacement Surgery performed?
Ankle replacement is usually performed under general or spinal anesthesia. The procedure involves:
-
Making an incision over the ankle to access the joint
-
Removing damaged cartilage and bone from the ankle joint
-
Positioning a metal and plastic implant to replicate normal ankle movement
-
Closing the incision with sutures and applying a protective dressing
The surgery typically takes 1-2 hours, depending on complexity and patient anatomy.
4. What is the recovery time after Ankle Replacement Surgery?
Recovery generally progresses as follows:
-
Immediate post-surgery: Patients may need a hospital stay of 1-3 days
-
First 6 weeks: The ankle is immobilized in a cast or boot; non-weight bearing is recommended
-
6-12 weeks: Gradual weight-bearing and physical therapy begin to restore strength and mobility
-
3-6 months: Most patients resume normal activities, though full recovery can take up to a year
Regular physical therapy is critical for regaining range of motion and joint function.
5. What are the benefits of Ankle Replacement Surgery?
The primary benefits include:
-
Pain relief from arthritis or joint degeneration
-
Improved ankle mobility compared to fusion surgery
-
Better walking ability and overall function
-
Preservation of adjacent joints, reducing the risk of secondary arthritis
Ankle replacement allows patients to perform daily activities with greater comfort and mobility.
6. What are the risks or complications of Ankle Replacement Surgery?
As with any major surgery, risks include:
-
Infection at the surgical site
-
Blood clots in the legs (deep vein thrombosis)
-
Implant loosening or failure over time
-
Nerve or blood vessel damage
-
Persistent pain or stiffness
Choosing a board-certified orthopedic surgeon and following post-operative care instructions minimizes complications.
7. How long does an ankle replacement last?
Modern ankle implants are designed to last 10-20 years, depending on factors such as:
-
Patient activity level
-
Weight and overall health
-
Implant type and surgical technique
Regular follow-ups allow your surgeon to monitor the implant and address any wear or complications early.
8. Can I walk normally after Ankle Replacement Surgery?
Yes. After rehabilitation and physical therapy, most patients can:
-
Walk without pain
-
Perform daily activities comfortably
-
Engage in low-impact activities like swimming, cycling, or walking
High-impact activities (running, jumping, or contact sports) are generally discouraged to protect the implant.
9. How should I prepare for Ankle Replacement Surgery?
Preparation steps typically include:
-
Medical evaluation including blood tests, X-rays, or CT scans
-
Medication review, including blood thinners or anti-inflammatory drugs
-
Pre-operative physical therapy to strengthen surrounding muscles
-
Arranging home support for the first few weeks after surgery
-
Stopping smoking to promote better healing
Your surgeon will provide a personalized preparation plan for optimal outcomes.
10. How is Ankle Replacement different from Ankle Fusion?
-
Ankle Replacement: Preserves joint movement and relieves pain. Ideal for patients who want to maintain mobility.
-
Ankle Fusion (Arthrodesis): Permanently fuses ankle bones, eliminating movement but providing pain relief. Recommended for patients with severe deformities or poor bone quality.
The choice between replacement and fusion depends on age, activity level, severity of joint damage, and overall health.


