Introduction to Decompressive Craniectomy
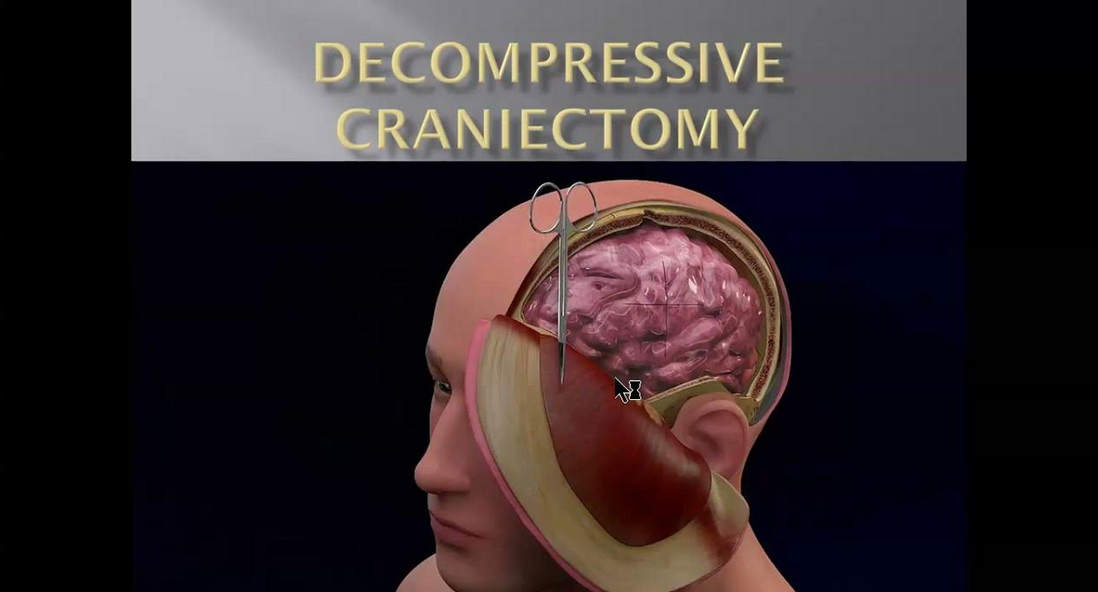
Decompressive craniectomy (DC) is a lifesaving neurosurgical procedure performed to reduce elevated intracranial pressure (ICP) that cannot be managed by medical means alone. The operation involves removing a section of the skull (bone flap) to allow the swollen brain to expand outward rather than being compressed within the rigid cranial cavity. This procedure is critical in preventing brain herniation, a condition where swelling pushes brain tissue downward through the skull base, leading to irreversible damage or death.
Under normal conditions, the brain, cerebrospinal fluid (CSF), and blood coexist within a closed skull at a delicate pressure balance. When trauma, stroke, infection, or hemorrhage causes swelling, the skull cannot expand. The result is a dangerous rise in ICP that reduces cerebral perfusion (blood supply to the brain), leading to ischemia (oxygen deprivation) and secondary neuronal death. Decompressive craniectomy gives the brain “room to breathe” by opening this closed compartment, relieving mechanical stress and restoring cerebral circulation.
Modern decompressive craniectomy techniques are supported by intensive neuro-monitoring, high-resolution imaging, and critical-care advances that improve patient outcomes. While the operation does not treat the initial cause of brain injury, it prevents secondary damage from pressure buildup and oxygen deprivation. The bone flap removed during surgery is either preserved in sterile freezing conditions or temporarily implanted in the abdominal wall, to be replaced later through a procedure called cranioplasty once the swelling has subsided.
In summary, decompressive craniectomy serves as a vital rescue therapy for patients suffering from life-threatening brain swelling due to traumatic brain injury, large ischemic stroke, intracerebral hemorrhage, or severe infection.
Causes and Risk Factors Leading to Decompressive Craniectomy
The primary reason for performing a decompressive craniectomy is raised intracranial pressure (ICP) caused by brain swelling. The causes may vary, but they all share the same underlying danger - the rigid skull restricts the expansion of swollen brain tissue, leading to compression of vital brain centers.
Major Causes
-
Severe Traumatic Brain Injury (TBI):
Traumatic brain injuries, often resulting from road accidents, falls, or sports injuries, are the most common indication for decompressive craniectomy. The trauma can cause bleeding (subdural, epidural, or intracerebral hematoma) and diffuse swelling (edema). This leads to rapid intracranial hypertension that, if uncontrolled, can cause brainstem compression and death. -
Massive Ischemic Stroke (Malignant Middle Cerebral Artery Infarction):
A large ischemic stroke can cause one hemisphere of the brain to swell dramatically. Known as “malignant MCA infarction,” it typically occurs within 48 hours of stroke onset. Decompressive craniectomy significantly reduces mortality in such cases by preventing midline shift and herniation. -
Intracerebral Hemorrhage:
Hypertensive crises, ruptured aneurysms, or blood vessel malformations can lead to intracerebral bleeding. The pooled blood exerts pressure on adjacent brain tissue. Removing the clot and decompressing the brain helps preserve function. -
Cerebral Venous Sinus Thrombosis (CVST):
In this condition, venous blockage leads to back-pressure and swelling in the brain tissue. Decompression is required when medical treatment fails to reduce swelling. -
Infectious or Postoperative Swelling:
Severe brain infections such as encephalitis or postoperative edema after tumor removal can cause life-threatening pressure rises requiring emergency decompression. -
Cerebellar Swelling or Posterior Fossa Lesions:
When swelling affects the back of the brain (posterior fossa), it can compress the brainstem - the control center for breathing and heartbeat. Posterior fossa decompression is performed in such cases.
Risk Factors that Increase the Need for Surgery
-
Delayed hospital admission or diagnosis after head trauma or stroke.
-
Coagulopathies or patients on anticoagulant therapy (risk of bleeding).
-
Uncontrolled hypertension leading to repeated microbleeds.
-
Hypoxia or low blood pressure after trauma, worsening brain injury.
-
Elderly patients with fragile vasculature and impaired autoregulation.
-
Diffuse brain edema on imaging, with little response to medication.
-
Metabolic disorders or diabetes, increasing the risk of ischemic swelling.
Decompressive craniectomy is typically considered a last-line intervention - used when hyperosmolar therapy, sedation, hyperventilation, and barbiturate coma fail to control intracranial pressure.
Symptoms and Signs Suggesting Decompressive Craniectomy
Patients who ultimately require decompressive craniectomy often present with symptoms of raised intracranial pressure or neurological deterioration.
Early Warning Symptoms
-
Persistent severe headache, especially after trauma or stroke.
-
Nausea and vomiting, often projectile and unrelated to meals.
-
Blurred vision or double vision due to pressure on the optic nerves.
-
Confusion, irritability, or restlessness.
-
Speech disturbances or difficulty concentrating.
Progressive and Severe Signs
-
Drowsiness or loss of consciousness (coma).
-
Unequal pupil sizes (anisocoria) - an indicator of pressure on cranial nerves.
-
Weakness or paralysis on one side (hemiplegia).
-
Seizures or abnormal posturing (decorticate/decerebrate).
-
Abnormal breathing pattern and slow pulse with high blood pressure - known as Cushing's Triad, a hallmark of dangerously high ICP.
Late Stage / Emergency Indicators
-
Fixed, dilated pupils indicating herniation.
-
Loss of brainstem reflexes (gag, corneal, pupillary).
-
Coma and respiratory failure requiring immediate mechanical ventilation and surgical decompression.
Rapid recognition and emergency imaging are essential to prevent irreversible damage.
Diagnosis and Preoperative Evaluation
Diagnosis involves clinical examination, neuroimaging, and intracranial pressure monitoring to confirm elevated ICP and determine surgical necessity.
Clinical Assessment
-
Detailed neurological evaluation using the Glasgow Coma Scale (GCS).
-
Assessment of pupillary reactions, limb strength, and cranial nerve function.
-
Vital signs monitoring for evidence of Cushing's triad.
Imaging Studies
-
CT Brain (Non-Contrast):
The gold standard for rapid diagnosis. It identifies bleeding, midline shift, brain swelling, compressed ventricles, and herniation signs. -
MRI Brain:
Provides detailed images of soft tissue injury, ischemic areas, and diffuse axonal damage. -
CT Angiography or Perfusion Imaging:
Used in stroke cases to identify blocked arteries and salvageable tissue. -
X-rays and Laboratory Tests:
Includes coagulation profile, electrolyte levels, and infection markers to guide surgery preparation.
ICP Monitoring
If the ICP exceeds 25 mmHg for more than 15-30 minutes despite maximal medical treatment, decompressive craniectomy becomes necessary.
Preoperative Preparation
-
Stabilize airway and breathing (intubation and ventilation).
-
Correct blood pressure, hydration, and electrolytes.
-
Control seizures and temperature.
-
Discuss surgical risks, benefits, and prognosis with family members.
Treatment Options and the Surgical Procedure
Treatment of wounds, burns, and infections can include both non-surgical and surgical interventions-ranging from cleaning and topical care to advanced surgical procedures like debridement, escharotomy, skin grafting, and reconstruction. The approach depends on wound type, burn depth, infection severity, and patient factors.
Surgical Techniques
There are several types of decompressive craniectomy, depending on the underlying cause and location of brain swelling:
-
Unilateral (Hemicraniectomy):
The most common type, performed when swelling is localized to one hemisphere (e.g., malignant MCA infarction). The bone flap typically measures 12-15 cm and covers the frontal, temporal, and parietal regions. -
Bifrontal Craniectomy:
Performed in diffuse brain swelling or bilateral frontal lobe injury. It involves removing both frontal bone plates to decompress the frontal lobes. -
Posterior Fossa Decompression:
Performed for cerebellar hemorrhages or posterior fossa swelling threatening the brainstem.
Step-by-Step Surgical Process
-
Anesthesia and Positioning:
The patient is placed under general anesthesia and positioned with the head stabilized to ensure proper access. -
Scalp Incision:
A large, question-mark-shaped incision is made behind the hairline for cosmetic healing. -
Bone Flap Removal:
Using a craniotome, the surgeon removes a bone segment. This flap is stored sterilely or in the abdomen for later cranioplasty. -
Dura Opening:
The dura mater is incised and expanded using a synthetic or pericranial patch (duraplasty) to prevent constriction. -
Hemostasis and Closure:
Bleeding is controlled, drains are placed, and the scalp is closed loosely to accommodate brain expansion. -
Bone Flap Preservation:
The bone is stored at -80°C or in the abdominal subcutaneous layer.
Postoperative Management
-
ICU care with ICP and cerebral perfusion monitoring.
-
Sedation, ventilation, and osmotic therapy (mannitol, hypertonic saline).
-
Regular CT scans to monitor brain relaxation.
-
Anticonvulsants for seizure prevention.
-
Antibiotics and wound care to prevent infection.
-
Early physiotherapy and limb mobilization once stable.
Prevention and Long-Term Management
While decompressive craniectomy is often an emergency, several strategies can reduce the likelihood of needing it.
Preventive Measures
-
Trauma prevention: Use helmets, seatbelts, and road-safety practices.
-
Stroke prevention: Control blood pressure, diabetes, and cholesterol.
-
Avoid smoking and alcohol abuse, both of which increase cerebrovascular risk.
-
Immediate care after head injury: Prompt CT imaging and hospitalization.
-
Infection control: Early treatment of meningitis or brain abscesses.
Postoperative Management
-
Maintain adequate oxygenation and hydration.
-
Monitor neurological recovery daily.
-
Prevent complications like pressure sores and infections.
-
Nutritional rehabilitation - high-protein, high-calorie diet.
-
Gradual transition from ICU to rehabilitation unit.
Complications of Decompressive Craniectomy
Despite being life-saving, DC is a major operation with potential complications:
Early Complications
-
Bleeding or hematoma formation.
-
Wound infection or meningitis.
-
Cerebral herniation through the bone defect.
-
Cerebrospinal fluid leak.
-
Seizures.
Late Complications
-
Hydrocephalus: Build-up of CSF, often requiring a ventriculoperitoneal shunt.
-
Subdural hygroma: Fluid accumulation beneath the dura.
-
Bone flap resorption or infection.
-
Syndrome of the Trephined: Neurological symptoms due to skull absence (fatigue, dizziness, cognitive changes).
-
Persistent motor or speech deficits.
With timely cranioplasty and multidisciplinary follow-up, many of these can be corrected or minimized.
Living with the Condition After Decompressive Craniectomy
Recovery after decompressive craniectomy is often long, gradual, and multidisciplinary.
Rehabilitation
-
Physical therapy to restore mobility and muscle strength.
-
Speech therapy for language or swallowing difficulties.
-
Occupational therapy to regain daily living skills.
-
Neuropsychological counseling for memory and emotional health.
Lifestyle and Daily Precautions
-
Wear a protective helmet until cranioplasty.
-
Avoid sports, heavy lifting, or falls.
-
Maintain strict medication compliance (antiepileptics, blood pressure control).
-
Attend regular neurologist and neurosurgeon visits.
-
Family members should provide emotional support and assist with care routines.
Cranioplasty Recovery
Cranioplasty - performed 3-6 months after DC - restores the skull's shape and protection. It improves cerebral blood flow and enhances cognition and aesthetics. Materials used include:
-
Autologous bone (original flap)
-
Titanium mesh
-
Polyetheretherketone (PEEK)
-
Acrylic or PMMA implants
Top 10 Frequently Asked Questions about Decompressive Craniectomy
1. What Is a Decompressive Craniectomy?
A decompressive craniectomy is a life-saving neurosurgical procedure in which a portion of the skull is temporarily removed to relieve excessive intracranial pressure (ICP) caused by brain swelling.
By creating space for the brain to expand safely, the procedure helps prevent brain damage, stroke, or death. The removed bone is usually stored and replaced later in a procedure called cranioplasty.
2. Why Is Decompressive Craniectomy Performed?
This procedure is performed in cases of dangerously high intracranial pressure that cannot be controlled by medication alone. Common indications include:
-
Severe traumatic brain injury (TBI)
-
Large ischemic or hemorrhagic stroke
-
Brain swelling due to infection or abscess
-
Post-surgical swelling after tumor removal
-
Severe brain edema that threatens neurological function
Its main goal is to protect brain tissue and preserve life.
3. How Is the Surgery Performed?
Decompressive craniectomy is performed under general anesthesia in an operating room with neurosurgical expertise.
Procedure Steps:
-
The scalp is carefully incised to expose the skull.
-
A section of the skull (bone flap) is removed to allow the brain to swell safely.
-
Swollen brain tissue is carefully managed, sometimes with dural opening to relieve pressure.
-
The scalp is closed over the exposed brain.
-
The removed bone flap is stored for later replacement (cranioplasty) once swelling subsides.
Surgery duration varies depending on injury severity.
4. What Are the Signs That Decompressive Craniectomy May Be Needed?
Dangerously high intracranial pressure can present with:
-
Severe headache or persistent vomiting
-
Decreased consciousness or drowsiness
-
Unequal or dilated pupils
-
Weakness or paralysis on one side
-
Seizures
-
Rapid deterioration in neurological function
Immediate medical evaluation is critical, as untreated elevated ICP can cause permanent brain injury or death.
5. Is Decompressive Craniectomy Painful?
During surgery, patients are under general anesthesia, so they feel no pain.
After surgery, mild discomfort, headache, or scalp tenderness is common. Pain is managed with analgesics, and intensive care monitoring ensures patient comfort during early recovery.
6. What Are the Risks or Complications?
While lifesaving, decompressive craniectomy carries risks:
-
Infection at the surgical site or meningitis
-
Bleeding or hematoma
-
Seizures
-
Brain tissue injury or ischemia
-
Cerebrospinal fluid leakage
-
Neurological deficits (depending on underlying brain injury)
These risks are minimized with expert surgical technique and intensive post-operative care.
7. How Long Does Recovery Take?
Recovery varies depending on the severity of the brain injury:
-
ICU stay: 3-10 days for close monitoring
-
Hospital stay: 2-4 weeks, longer if complications arise
-
Rehabilitation: Physical, occupational, and speech therapy may be required for weeks to months
-
Cranioplasty (bone replacement): Usually performed 6-12 weeks after initial surgery
Full neurological recovery may take several months to a year, depending on injury severity.
8. Who Is a Good Candidate for Decompressive Craniectomy?
Candidates include patients with:
-
Life-threatening brain swelling not responding to medical treatment
-
Severe traumatic brain injury
-
Large ischemic or hemorrhagic stroke causing elevated ICP
-
Brain edema following infection or surgery
This procedure is generally reserved for emergency situations where immediate pressure relief is necessary to save life.
9. What Is the Difference Between Decompressive Craniectomy and Craniotomy?
-
Craniotomy: Bone flap is temporarily removed and replaced during the same surgery.
-
Decompressive Craniectomy: Bone flap is temporarily removed and stored, allowing the brain to swell without compression, and replaced later (cranioplasty).
Craniectomy is typically used in emergency, high-risk swelling situations, whereas craniotomy is used for planned surgeries like tumor removal.
10. What Is the Long-Term Outlook After Decompressive Craniectomy?
The long-term prognosis depends on:
-
Severity of the initial brain injury or swelling
-
Age and overall health
-
Timing of surgery and post-operative care
Many patients survive life-threatening conditions and regain functional
independence, although some may experience residual neurological
deficits.
Rehabilitation and cranioplasty help restore quality of life and
protect the brain long-term.


