What is Spider Veins?

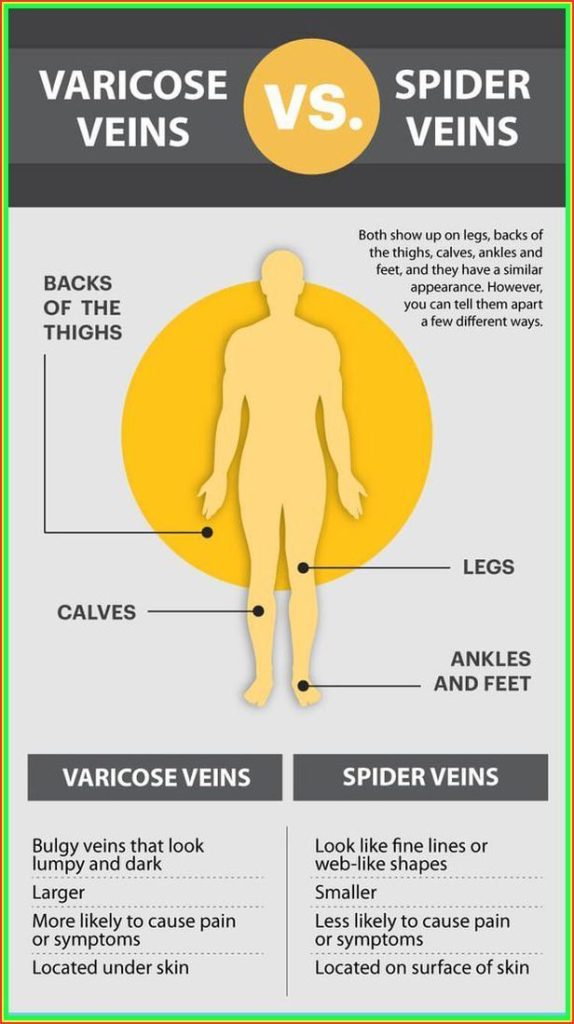
Spider veins, also known as telangiectasia, are small, damaged blood vessels visible just beneath the skin’s surface, typically appearing as red, blue, or purple lines, webs, or branches. While usually harmless, they may cause mild discomfort such as burning or itching, especially in the legs. Treatment options include sclerotherapy, laser therapy, or lifestyle changes. Varicose veins, on the other hand, are larger, swollen veins that often appear blue or dark purple, commonly found on the legs, and can cause discomfort or complications. Treatment for varicose veins may involve surgery or minimally invasive procedures like endovenous thermal ablation. Both spider and varicose veins can be treated for cosmetic reasons or to alleviate symptoms and prevent complications.
What are the causes of Spider Veins?
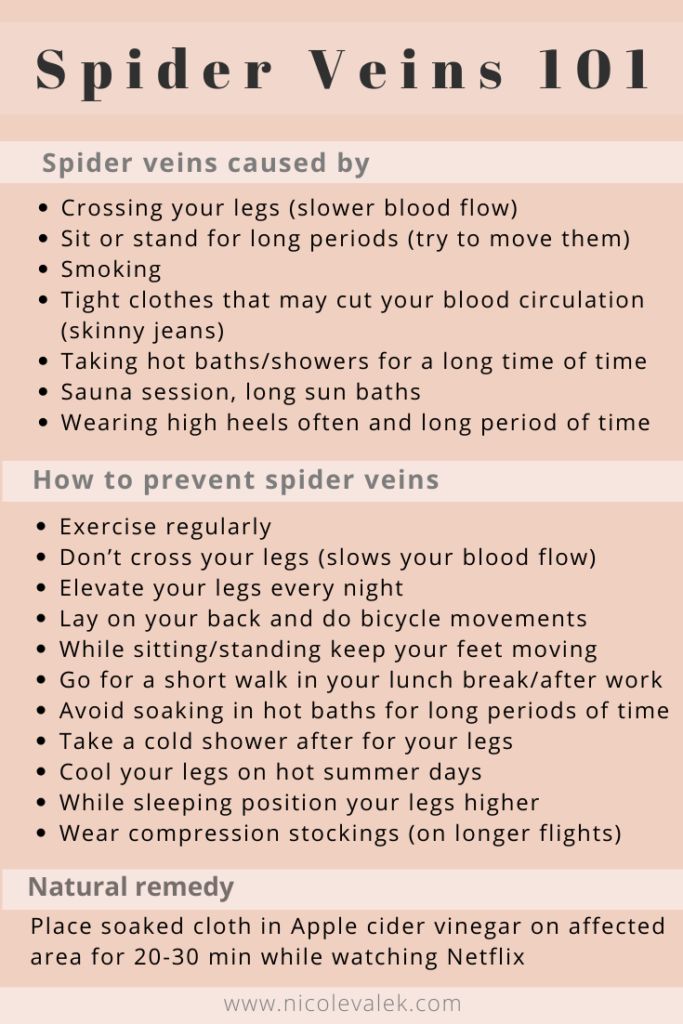
Spider veins form when the small blood vessels just under the skin weaken and expand, leading to their visible appearance. The exact causes of spider veins are not always clear, but several factors may contribute to their development:
- Hormonal changes: Fluctuations in hormone levels, such as those occurring during puberty, pregnancy, breastfeeding, or menopause, can contribute to the development of spider veins.
- Genetic syndromes: Spider veins may run in families, suggesting a genetic predisposition to the condition.
- Connective tissue diseases: Certain connective tissue disorders can weaken blood vessels and contribute to the formation of spider veins.
- Injury or trauma: Trauma or injury to the skin or veins, particularly in the legs, can lead to the development of spider veins.
Spider veins on the face may result from tiny blood vessels bursting due to increased pressure or sun damage.
Similarly, the causes of varicose veins are not fully understood, but several factors may increase the risk of developing them:
- Family history: Varicose veins often run in families, indicating a genetic component to the condition.
- Hormonal factors: Changes in estrogen levels, such as those occurring during puberty, pregnancy, or menopause, may contribute to the development of varicose veins, with women being more affected than men.
- Prolonged standing or sitting: Jobs or activities that involve prolonged periods of standing or sitting can increase pressure on the veins, potentially leading to varicose veins.
- Lack of exercise: Inactivity can impair circulation and increase the risk of developing varicose veins.
- Obesity: Excess weight can put additional pressure on the veins, increasing the likelihood of varicose vein development.
- Other factors: Conditions such as chronic venous insufficiency, pregnancy, constipation, and tumors (in rare cases) can also contribute to the development of varicose veins.
Spider veins and varicose veins are common conditions, with a significant proportion of the population affected, particularly women and individuals over the age of 50. Understanding the factors that contribute to their development can help in prevention and management strategies.
What are the symptoms of spider veins?
Symptoms of Spider Veins:
- Spider veins often have no symptoms beyond their undesirable appearance.
- However, they can sometimes cause discomfort, including swelling, throbbing, and restless legs.
- They may become painful and lead to skin issues such as discoloration, skin ulcers, or blood clots, especially after prolonged sitting or standing.
- Common symptoms include a general uncomfortable feeling in the legs, rash, cramping or aching, and itching around the veins.
Common Symptoms of Spider Veins:
- Heaviness or Aches: Feeling of heaviness or aching, particularly in the legs.
- Burning, Cramps, or Swelling: Burning sensation, swelling, and muscle cramps may occur.
- Increased Pain After Prolonged Sitting or Standing: Pain often worsens after remaining in one position for an extended period.
- Itching: Itching sensation under the skin, sometimes accompanied by skin inflammation.
- Skin Discoloration: Enlarged veins may cause skin discoloration around the affected area.
What are the Risk Factors?
Risk factors for Spider Veins:
- Prolonged standing or sitting
- Family history of spider veins or varicose veins
- Obesity (BMI > 30)
- Pregnancy
- Use of hormonal birth control or hormone therapy for menopause
- Excessive sun exposure
- Smoking or history of smoking
- Genetics (up to 90% of people with spider veins have a family history)
- Pregnancy (increased blood flow and weight of the fetus can strain leg veins)
- Gender (females are more affected, especially during menopause)
- Aging (weakening of vein valves and calf muscles over time)
- Overweight or obesity
- Hormonal factors (birth control pills or hormone therapy)
- Prolonged sitting or standing
- History of blood clots or vein damage
- Excessive pressure in the face (from coughing, sneezing, vomiting, etc.)
- Sun damage to the skin
Additionally, pregnancy is a significant risk factor for both spider veins and varicose veins due to increased blood volume, hormonal changes, and pressure on pelvic veins as the uterus grows. While varicose veins may improve after pregnancy, they may not completely disappear, and some may remain visible.
Understanding these risk factors can help individuals take preventive measures and seek appropriate treatment if needed to manage spider veins and varicose veins effectively.
What are the Complications?
- Spider veins on their own rarely cause complications, but when combined with conditions like Chronic Venous Insufficiency (CVI), they can increase the risk of venous stasis ulcers or cellulitis.
- It’s crucial to monitor for signs of complications and communicate any concerns with a healthcare provider.
- While spider veins are primarily seen as a cosmetic issue, they can sometimes lead to discomfort and complications, especially in those with underlying health conditions.
- Regular monitoring and seeking medical advice when necessary are important for effectively managing spider veins.
How can I prevent it?
- Healthy Diet: Eating a diet rich in fiber and low in sodium can help maintain a healthy weight and reduce the risk of developing or worsening spider veins. A diet high in fiber supports good digestion, which in turn promotes healthy blood flow.
- Hydration: Drinking plenty of water throughout the day can help keep blood vessels hydrated and functioning optimally. Proper hydration also supports overall circulation.
- Regular Movement: Incorporating regular movement throughout the day, such as taking short walks or stretching breaks, can help prevent blood from pooling in the legs and reduce the risk of developing spider veins.
- Avoiding Prolonged Crossed Legs: Sitting with crossed legs for extended periods can restrict blood flow and increase pressure on veins, contributing to the development of spider veins. Keeping both feet flat on the ground while sitting can help maintain healthy circulation.
- Leg Exercises: Performing specific leg exercises, such as ankle circles, calf raises, and leg lifts, can help strengthen the muscles that support healthy blood flow in the legs.
- Stress Management: Chronic stress can contribute to poor circulation and may exacerbate vein-related issues. Practicing stress-reducing techniques such as deep breathing, meditation, or yoga can help promote relaxation and support overall vein health.
- Proper Footwear: Wearing comfortable, supportive shoes can help promote healthy circulation and reduce the risk of developing vein-related problems in the feet and legs.
- Regular Check-ups: Regular visits to a healthcare provider can help monitor vein health and identify any potential issues early on. They can also provide personalized advice and treatment options if needed.
What are the Treatments of Spider Veins?
- Support (Compression) Stockings: These apply gentle pressure to the legs, preventing blood pooling and reducing swelling.
- Lifestyle Changes: This includes maintaining good skin hygiene, weight management, regular exercise, avoiding prolonged sitting or standing, wearing low-heeled shoes, and elevating legs when resting.
- Sclerotherapy: Injection of a solution into the vein, causing it to collapse and fade over time.
- Endovenous Laser Ablation: Laser energy is used to heat and collapse the affected vein.
- Radiofrequency Occlusion: Radiofrequency energy is applied to the vein wall, causing it to collapse and seal shut.
- Surgery: Options include ligation and stripping, endoscopic vein surgery, and ambulatory phlebectomy.
- Laser Treatment: Strong bursts of light are directed onto the spider veins, causing them to fade.
- Catheter-Based Procedures: Radiofrequency or laser energy is used to seal the vein shut.
Treatments specifically for Spider Veins:
- Sclerotherapy: Injection of a sclerosant solution directly into the targeted vein, causing it to collapse and fade.
- Compression Stockings: These improve circulation by applying pressure to the legs, reducing swelling and preventing new spider veins.

Preventive Measures:
- Sun Protection: Limiting sun exposure and wearing sunscreen can prevent spider veins, especially on the face.
- Avoiding Heat Exposure: Extreme heat from weather, saunas, and hot tubs can increase blood vessel dilation.
- Moderate Alcohol Consumption: Excessive alcohol consumption can contribute to broken blood vessels on the face.
- Protective Gear: Wearing face gear and helmets during activities can reduce injuries and prevent spider veins.
- Maintaining Healthy Habits: Regular exercise, reaching a moderate body weight, and avoiding prolonged standing or sitting can help prevent varicose veins from worsening.
- Over-the-counter treatments: There are various topical creams and emollients available to soothe pain and discomfort associated with varicose veins.
- Following Treatment Plans: Individuals undergoing treatment for conditions like rosacea should stick to their plans and consult their doctors if necessary.